Inhalant Use Disorder – What It Is, Symptoms & Treatment

In this article
Inhalant use disorder is a reality. It is a condition where daily functioning, relationships, and one’s own health are interrupted through repeated use of intoxicants. Inhalants are commonly used drugs made up of volatile substances. They are used to get a rapid, mood-altering effect.
Long-term, systemic use over an extended period can produce mental and physical harm. It alters behavior, thought, and emotional control. Symptoms vary from mild to severe issues. Its danger is increased when taken daily or for an extended period of time. For those seeking a safe space to talk and begin healing, Calmerry offers access to compassionate online therapy that fits individual needs. Early intervention exists, and harm is avoided through knowledge of warning behaviors, medical effects, and treatment.
What is inhalant use disorder?
Inhalant addiction can develop from occasional use to compulsive inhalation, often starting in adolescence due to easy access. Intoxicants include household and industrial products like solvents, aerosols, gases, and nitrites. These are not intended for human use but can alter mood or perception when inhaled.
This substance disorder may involve repeated use that disrupts daily life. Inhaled chemicals reach the brain within seconds, creating quick effects that encourage continued use and increase the risk of lasting brain, organ, and cognitive damage.
According to DSM-5 guidelines, inhalant use disorder is defined by harmful patterns of use, related symptoms, and reduced functioning, regardless of the specific substance.
Health risks range from immediate dangers like overdose to long-term damage to the brain, lungs, heart, and other organs.
What is the prevalence of inhalant use disorder?
Volatile substance use disorder primarily affects younger people, particularly adolescents and teens. Inhalant use remains most common in early teen years, with its prevalence declining in older age groups. In specialized settings like juvenile justice systems, a significant portion of youth who have used inhalants meet criteria for abuse or dependence. [1] Howard, M. O., & Perron, B. E. (2009). A Survey of Inhalant Use Disorders among Delinquent Youth: Prevalence, Clinical Features, and Latent Structure of DSM-IV Diagnostic Criteria. BMC Psychiatry, 9(1). https://doi.org/10.1186/1471-244x-9-8
Though likely underreported, these patterns suggest that substance use disorder affects vulnerable youth disproportionately, highlighting the need for focused prevention and treatment efforts.
Inhalant abuse statistics
Reports from U.S. surveys show a steady decline in inhalant use. In 2023, under 1 % of people aged 12 and older reported using inhaled chemicals in the past year. [2] Inhalants. (2024, September 18). National Institute on Drug Abuse. https://nida.nih.gov/research-topics/inhalants Among younger teens, the 2022 Monitoring the Future study recorded approximately 3.6 % of 8th graders reporting intoxicant use. [3] Miller, J. (2025, June 22). Inhalant Addiction statistics – Inhalant abuse demographics (2025). AddictionHelp.com. https://www.addictionhelp.com/inhalants/statistics/ In 2025, 1 in 5 students in another national survey admitted trying inhaled chemicals at least once, while 7 % had used them in the prior month. [4] Inhalants and young people – Alcohol and Drug Foundation. (n.d.). https://adf.org.au/insights/inhalants-young-people/
What are the symptoms of inhalant exposure?
Inhalant exposure can cause a combination of physical symptoms, behavioral shifts, and emotional disturbances. These may appear quickly or develop over time, depending on the duration and intensity of use. Common signs include:
- Persistent chemical odors on breath or clothing
- Noticeable paint or solvent stains on hands, fingers, or clothes
- Marked behavioral changes, such as apathy or loss of motivation
- Significant reduction in appetite with visible weight loss
- Abrupt change in friends and preferred hobbies
- Rapid decline in school or academic performance
- Neglect of personal hygiene and grooming habits
- Slurred or slow speech patterns
- Frequent runny nose or unexplained nosebleeds
- Constant or unexplained fatigue and low energy
- Ulcers, sores, or irritation around the nose and mouth
- Periods of confusion and reduced concentration
- Ongoing depression, irritability, hostility, or emerging paranoia
What are the risk factors for inhalant use disorder?
Risk factors for volatile substance use often emerge from a mix of personal, social, and environmental influences. Early onset of inhalant use during adolescence can increase vulnerability, especially when paired with limited awareness of the health effects or consequences.
A history of inhalant use, substance abuse, or other substance use disorders may heighten susceptibility. Mental health conditions, including depression, anxiety, or antisocial personality disorder, can also contribute.
Unstable living conditions and peer influence may encourage repeated use of intoxicants. Limited access to support networks and healthy recreational activities further increases the likelihood of misuse or dependence.
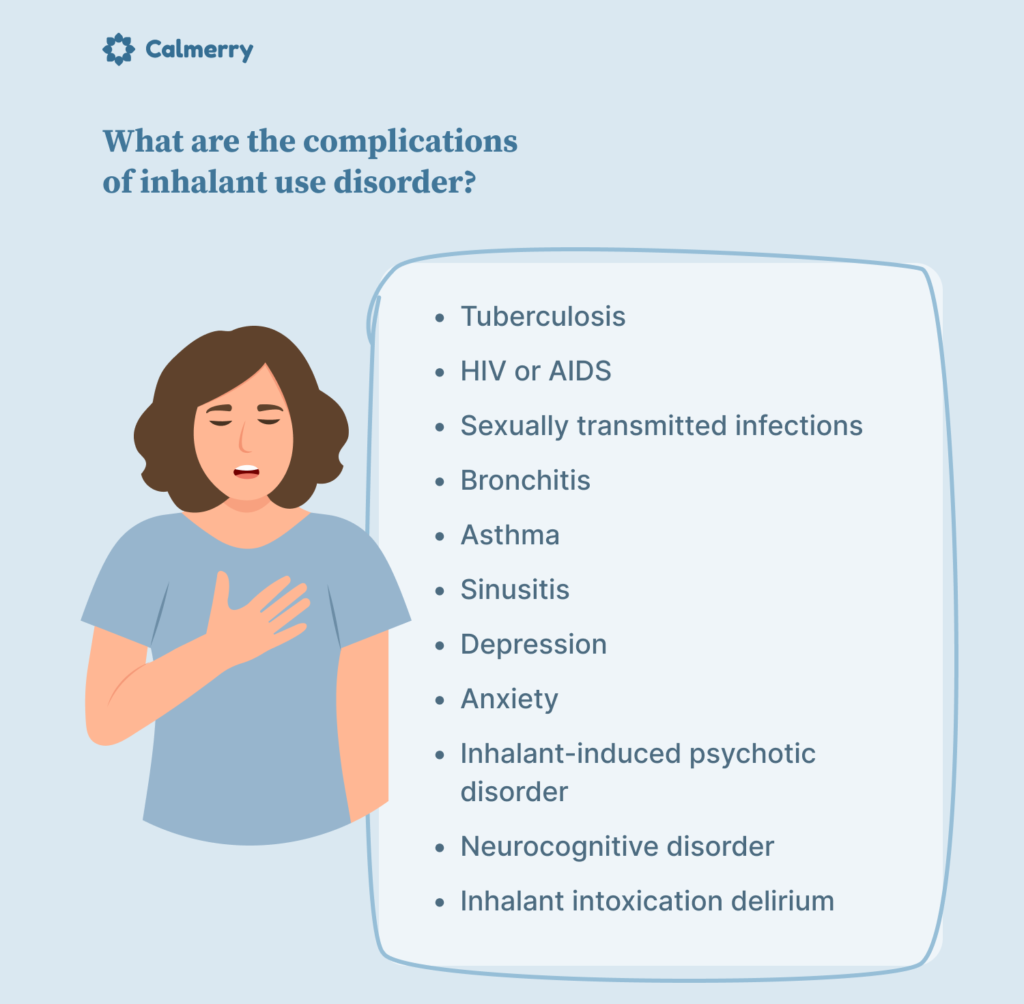
What are the complications of inhalant use disorder?
Complications from inhalant use disorder can affect both physical and mental health, sometimes leading to long-term impairment. Continuous inhalation of volatile substances can damage the respiratory, cardiovascular, and nervous systems, while also increasing vulnerability to infections and psychiatric conditions. Possible complications are the following:
- Tuberculosis
- HIV/AIDS
- Sexually transmitted infections
- Bronchitis
- Asthma
- Sinusitis
- Depression
- Anxiety
- Inhalant-induced psychotic condition
- Major or mild neurocognitive condition
- Inhalant intoxication delirium
How is inhalant use disorder diagnosed?
Diagnosis of substance use disorder from inhalants calls requires a detailed clinical evaluation. The evaluation is carried out on the physical and behavioral use patterns of inhaled substances. A physician determines a medical and mental health history. Patterns of substance use and physical or cognitive changes that are connected to them are also reviewed by them.
The evaluation process typically involves specialized interviews and periodic evaluation measures. They aid in the identification of evidence concerning abuse of intoxicants, withdrawal, or dependency. Such evidence regarding changes in behavior, poor balance, and memory problems is accorded special attention. Accurate diagnosis guides treatment planning and is sensitive to associated diseases that affect general well-being.
How is inhalant use disorder treated?
Treatment for inhalant use disorder focuses on breaking the cycle of repeated use and addressing the psychological, behavioral, and social factors that contribute to dependence. Approaches often include:
- Cognitive behavior therapy (CBT): Helps individuals identify and change harmful thought patterns linked to inhalant addiction.
- Motivational interventions: Encourage readiness to stop using the substance and set personal goals for recovery.
- Family counseling: Strengthens support systems and improves communication.
- Activity and engagement programs: Promote healthy routines and meaningful participation in daily life.
- Support groups and 12-step programs: Provide community, accountability, and shared experiences for ongoing recovery.
Can a person overdose on inhalants?
A person can experience an overdose, which happens when the inhalation of volatile substances overwhelms the body’s ability to process them. High concentrations can disrupt heart rhythm, impair breathing, and affect the central nervous system, leading to loss of consciousness or sudden death.
The effects of inhalant overdose may also include seizures, severe confusion, and dangerous drops in blood pressure. Any suspected overdose requires immediate medical attention, as even a single use in high amounts can be fatal. Prompt intervention can reduce the risk of long-term damage to physical and mental health.
Diagnosis of inhalant use disorder
Identifying this use disorder requires a clear understanding of the individual’s patterns of behavior, substance use, and overall mental health. A professional assessment can determine the severity of intoxicant addiction, the presence of co-occurring conditions, and the most appropriate next steps for care.
Clinical evaluation and history – Reviewing the person’s history of inhaled toxin use, related health effects, behavioral changes, and any previous substance abuse or dependence concerns.
Diagnostic tools and assessment criteria – Applying established diagnostic guidelines, structured interviews, and symptom checklists to confirm the substance use disorder and guide treatment planning.
Treatment options
Effective recovery from inhalant use disorder often requires a structured approach that addresses both the physical and mental health challenges linked to repeated use of intoxicants. Interventions may include:
- Behavioral therapy (CBT, motivational interviewing): Helps identify harmful patterns, develop healthier coping skills, and reduce the risk of relapse.
- Support groups and family involvement: Strengthen social connections and provide consistent encouragement during recovery.
- Inpatient vs outpatient care: Offers varying levels of supervision and therapeutic intensity based on individual needs.
- Addressing co-occurring disorders: Treats conditions such as depression, anxiety, or antisocial personality disorder alongside inhaled toxin addiction.
Can inhalant use disorder be prevented?
Preventing inhalant use disorder involves strengthening protective factors that reduce vulnerability to substance abuse. Positive self-image, supportive relationships, and healthy coping skills can help reduce the likelihood of experimenting with or repeatedly using inhalants.
- Increasing self-esteem and communication, boosting confidence, and promoting open dialogue within families, schools, and communities.
- Improving personal relationships – building trust, respect, and emotional support in social and family networks.
- Managing anxiety and pressure – developing healthy stress management techniques, such as physical activity, creative outlets, or relaxation practices.
What is the prognosis for inhalant use disorder?
The prognosis for inhalant use disorder varies widely and depends on multiple personal and treatment-related factors. Recovery outcomes improve when the condition is recognized early and addressed with consistent support. Key elements that influence prognosis include:
- The severity of the disorder – more advanced cases may require longer, intensive care.
- The degree of dependence – stronger dependence can complicate recovery.
- The level of commitment to quitting – sustained motivation supports lasting change.
- Treatment time frame – adequate duration helps reinforce progress.
- How you handle stressful situations – effective coping strategies reduce relapse risk.
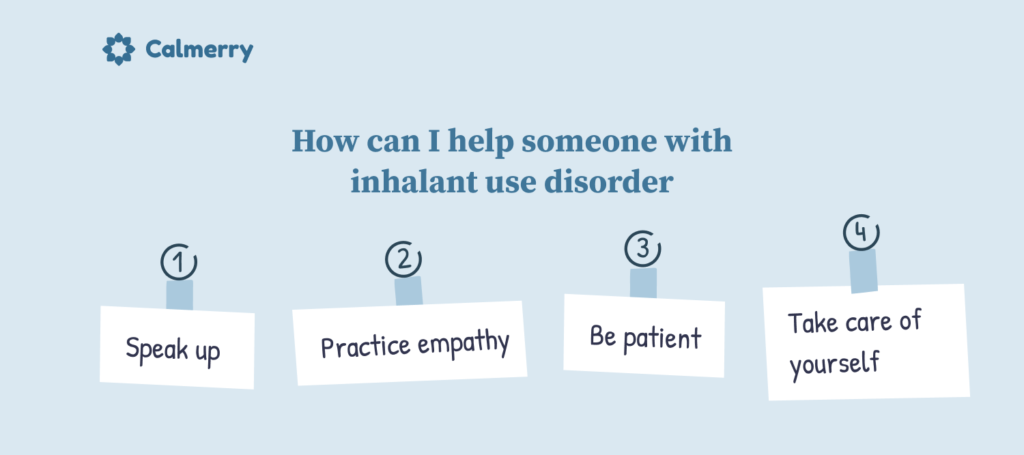
How can I help a loved one with inhalant use disorder?
Treating a substance disorder patient is a task that needs persistent attention and intentional actions. Compassionate attitudes can create trust and inspire the patient to embrace support.
- Speak up for oneself – Express concerns clearly and briefly, with what one has noticed, without judging.
- Practice empathy – Practice empathizing towards their struggles and emotions, even when you’re not entirely sure about their choices.
- Be patient – Recovery from volatile substance dependency can be a slow process, and the journey towards recovery can be gradual.
- Take care of your own well-being – be responsible for your own mental and physical well-being, and be a sustainable support to others.
Conclusion
Inhalant use disorders pose serious challenges to physical and mental health. This is especially true for vulnerable groups, like adolescent users. The effects go beyond just immediate intoxication. They include risks of long-term brain damage, respiratory issues, and emotional instability.
Recovery needs a structured approach. It should tackle both the physical effects of inhaling volatile substances and the psychological patterns related to use. Many people must manage withdrawal symptoms and understand how drug use impacts their health.
With steady support, evidence-based treatment, and strategies to lower risk and exposure, individuals can achieve better outcomes. They can also work toward lasting recovery.
FAQ
What is inhalant use disorder?
Inhalant use disorder is a type of substance use disorder that involves the repeated use of inhalants, volatile substances that produce chemical vapors. These vapors can alter mood, perception, and behavior. The condition is marked by patterns of abuse or dependence that can harm physical and mental health, daily functioning, and relationships.
Which substances are considered inhalants?
Inhalants include a wide range of products such as glues, paint thinners, gasoline, aerosol sprays, cleaning solvents, and nitrites. They contain chemicals that can be misused through the inhalation of volatile substances, often producing short-lived psychoactive effects but serious health risks.
Who is most at risk of developing inhalant use disorder?
Adolescents are more likely to begin inhalant use due to ease of access and low cost, but intoxicant addiction can affect people of any age. Individuals with a history of intoxicant use, other substance abuse, certain mental health conditions, or antisocial personality disorder may be at higher risk.
What are the signs that someone might be abusing inhalants?
Warning signs can include chemical odors on the breath or clothing, paint or stains on the skin, sudden changes in behavior or mood, poor concentration, and a decline in school or work performance. Physical symptoms of intoxicant abuse may include slurred speech, a runny nose, nosebleeds, fatigue, or ulcers around the mouth and nose.
Can inhalant use cause long-term damage?
Yes. Beyond getting high, the use of inhalants can have serious consequences. It can cause brain damage, hearing loss, organ failure, and long-term respiratory issues. Prolonged use of intoxicants can cause damage to the nervous system and organs.
Is Inhalant use disorder treatable?
Yes, it can be treated with well-crafted interventions. With proper help, most of those who inhale toxins can be treated and gain excellent physical and mental well-being. Treatment can include behavioral therapies, counseling, and treatment of co-occurring disorders.
What types of treatment are available for inhalant use disorder?
Effective treatment often combines CBT, motivational interventions, family counseling, activity-based programs, and peer support. Treatment can be delivered in outpatient or inpatient settings, depending on the severity of the substance use disorder and the presence of other substance use or mental health concerns.
Can inhalant use be fatal?
Yes. A single use of an inhaled chemical can cause sudden death from cardiac arrest, suffocation, or inhalant overdose. Long-term abuse of inhalants also raises the risk of fatal complications due to cumulative damage to the heart, lungs, and brain. Immediate medical attention is critical if an inhalant overdose is suspected.
How can I help someone who may be struggling with inhalant use?
Express concern directly, encourage them to seek professional help, and offer to support them in accessing treatment. Be patient and maintain empathy, as recovery from substance use disorder often requires time and persistence.
How can inhalant abuse be prevented?
Prevention can involve building self-esteem, strengthening personal relationships, and improving coping skills for stress and anxiety. Education about the dangers of intoxicants and limiting access to products that can be misused are also important.
How can Calmerry help?
Calmerry offers access to licensed mental health professionals who can provide assessment, therapy, and ongoing support for those struggling with substance use, including inhalant use disorder. Online counseling can help address both the psychological aspects of this addiction and the emotional challenges that accompany recovery.
Howard, M. O., & Perron, B. E. (2009). A Survey of Inhalant Use Disorders among Delinquent Youth: Prevalence, Clinical Features, and Latent Structure of DSM-IV Diagnostic Criteria. BMC Psychiatry, 9(1). https://doi.org/10.1186/1471-244x-9-8
Inhalants. (2024, September 18). National Institute on Drug Abuse. https://nida.nih.gov/research-topics/inhalants
Miller, J. (2025, June 22). Inhalant Addiction statistics – Inhalant abuse demographics (2025). AddictionHelp.com. https://www.addictionhelp.com/inhalants/statistics/
Inhalants and young people – Alcohol and Drug Foundation. (n.d.). https://adf.org.au/insights/inhalants-young-people/
online therapy
live video session