Insomnia and Addiction: Is There a Link?
In this article
Insomnia is a common sleep disorder that affects millions of people worldwide, often leading to serious health complications when left untreated. Its impact is even more profound when intertwined with substance addiction, creating a vicious cycle that disrupts the quality of rest and hinders recovery.
Understanding the relationship between addiction and sleeplessness is essential for effective treatment planning, especially when both conditions co-occur. This article explores causes, effects, and treatment options for this dual challenge, and how Calmerry can support people on their journey toward better sleep and recovery.
What is insomnia?
Insomnia is a common sleep disorder that affects the ability to fall or stay asleep, or achieve restorative rest, even when the opportunity is present. People with sleeplessness often experience sleep deprivation, leading to impaired daytime functioning, fatigue, irritability, and concentration problems. The insomnia symptoms may occur independently or as part of other physical or psychological conditions. [1] Robards, K. (2023, July 27). Understanding the relationship between sleep deprivation and addiction. Sleep Education. https://sleepeducation.org/understanding-relationship-between-sleep-deprivation-addiction/
Research from the American Academy of Sleep Medicine highlights that sleeplessness can be both a disorder and a symptom of other health problems, such as depression or anxiety. [2] International Classification of Sleep Disorders, 2nd Edition. (n.d.). Insomnia. https://aasm.org/resources/factsheets/insomnia.pdf
The connection between insomnia and addiction
The relationship between addiction and insomnia is complex and bidirectional. Sleeplessness can increase vulnerability to substance addiction, while chronic substance abuse can disrupt bedtime regulation. Individuals often turn to drugs or alcohol in an attempt to manage persistent sleep issues, leading to dependency over time.
Substance use disorder is frequently linked to disrupted sleep cycles, making it harder to achieve restful sleep without external substances. Over time, this can worsen both conditions.
Types of insomnia
- Short-term insomnia (also called acute insomnia) often follows stressful events or environmental disruptions and may contribute to the early stages of marijuana addiction and insomnia cycles.
- Chronic insomnia persists for months and is frequently associated with underlying mental health conditions such as anxiety or depression.
- Primary insomnia develops independently of other conditions and may lead to long-term effects of sleeplessness, like mood instability and fatigue.
- Secondary insomnia results from another medical or psychiatric issue, including alcohol addiction and insomnia, which frequently co-occur and intensify each other.
How addiction disrupts sleep
Substance addiction alters brain chemistry involved in sleep regulation, often leading to persistent sleep deprivation and poor rest architecture. Individuals with insomnia and sleeping pill addiction may rely on sedatives that eventually reduce natural sleep drive and worsen rebound sleeplessness. Without addressing the root causes, both bedtime issues and dependency can spiral, complicating the recovery process.
How insomnia contributes to addiction
When left untreated, the signs of insomnia, such as difficulty falling asleep or staying asleep, can drive individuals to self-medicate with drugs or alcohol. Without early intervention or appropriate symptoms and treatment options, this pattern may lead to dependency and complicate long-term recovery.
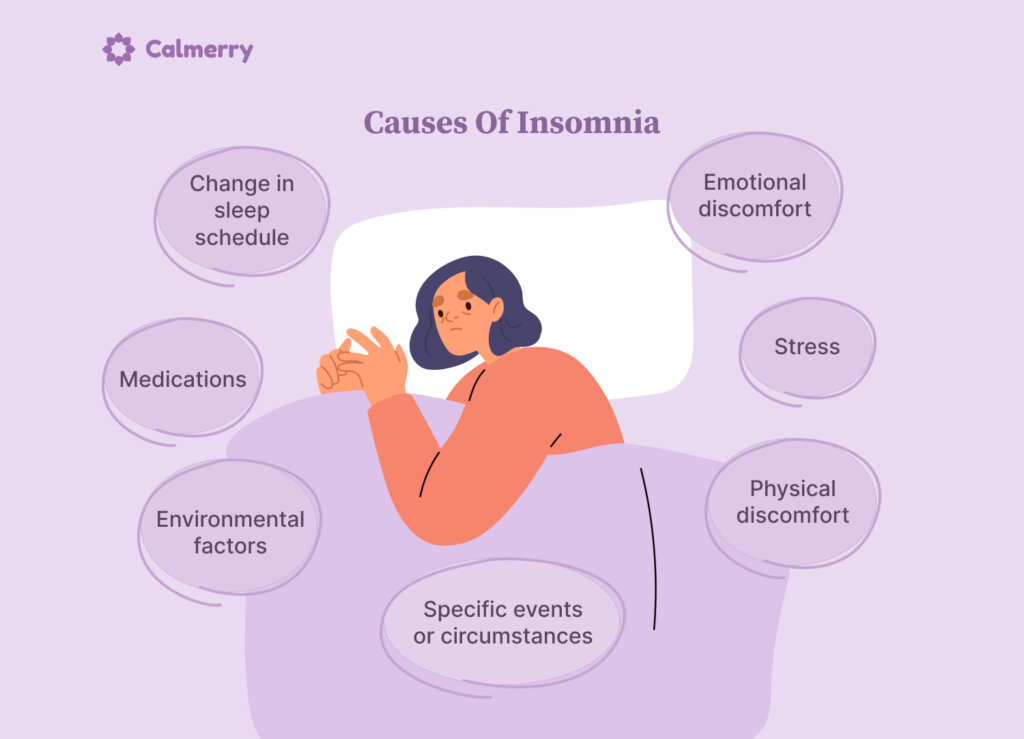
Causes of insomnia
- Stress from work or personal life can overstimulate the nervous system and delay sleep onset.
- Emotional discomfort, including anxiety or grief, often disrupts the ability to relax at night.
- Physical discomfort, such as pain or chronic illness, interferes with sustained sleep.
- Environmental factors like noise, light, or an uncomfortable mattress can prevent restful sleep.
- Medications, including stimulants or corticosteroids, may cause unwanted wakefulness.
- A change in sleep schedule from travel or shift work can disrupt circadian rhythms.
- Specific events or circumstances, such as trauma or major life changes, can trigger temporary sleeplessness.
Chronic insomnia causes
Chronic sleeplessness is diagnosed when disrupted rest patterns persist for at least 3 nights a week for at least 3 months. Below are some of the most common contributors:
- Chronic stress overstimulates the nervous system, making it difficult to unwind at night.
- Mental health disorders like anxiety or depression often disrupt natural sleep cycles.
- Physical health disorders, including chronic pain or respiratory conditions, can interfere with sustained rest.
- Substance use alters brain chemistry, contributing to long-term sleep disturbances.
- Poor sleep habits, such as irregular schedules or screen use before bed, weaken sleep quality over time.
- Hormonal changes, especially during menopause or thyroid imbalance, may trigger persistent wakefulness.
What is a dual diagnosis of insomnia and addiction?
A dual diagnosis refers to the co-occurrence of sleeplessness and a substance use disorder, where both conditions interact and exacerbate each other. Successful rehab treatment must address both sleep dysfunction and addiction simultaneously to improve outcomes.
The cycle of addiction and insomnia
Sleeplessness and addiction are often intertwined in a self-perpetuating cycle. One condition worsens the other, making it harder for individuals to break free without targeted support. Here’s how the cycle typically unfolds:
- Addiction and sleeplessness reinforce each other, creating a loop that’s hard to break.
- Ongoing sleep deprivation weakens emotional regulation, making cravings and withdrawal harder to manage.
- Continued substance use disrupts natural sleep cycles, preventing long-term sleep recovery.
- Integrated rehab treatment that targets both conditions is essential to stop the cycle and support healing.
Why do insomnia and addiction occur so often?
Insomnia and addiction frequently co-occur because both can stem from shared factors like chronic stress, trauma, or mental health conditions. Their overlap often creates a reinforcing cycle, where disrupted sleep increases vulnerability to substance use, and substance use worsens sleep disturbances.
Insomnia leading to addiction
Persistent insomnia can push individuals to misuse substances like alcohol, cannabis, or sedatives in an attempt to improve sleep, increasing the risk of substance use disorder. Over time, reliance on these substances reinforces unhealthy sleep behaviors and can escalate into full substance addiction.
Addiction leading to insomnia
Addiction disrupts the brain’s natural sleep-wake cycle, making it difficult to achieve restful sleep without substances. Even during treatment, withdrawal symptoms and neurochemical imbalances can prolong insomnia and delay sleep recovery.
How can I get help for insomnia and addiction?
Professional support often begins with a dual-diagnosis evaluation followed by personalized rehab treatment that addresses both sleep and substance issues. Since chronic sleeplessness is diagnosed based on persistent patterns, early medical consultation is key to tailoring effective recovery plans.
Insomnia and addiction treatment
Effective treatment for those co-occurring conditions requires an integrated approach that addresses both conditions at once.
- Cognitive Behavioral Therapy for Insomnia (CBT-I) targets unhelpful thoughts and behaviors that disrupt sleep without relying on substances.
- Sleep hygiene education promotes consistent routines and habits to improve sleep naturally.
- Dual diagnosis care addresses both insomnia and addiction simultaneously to prevent relapse.
- Medication (with caution) may be prescribed short-term, especially when chronic sleeplessness is diagnosed, but it is closely monitored to avoid dependency.
- Holistic approaches like mindfulness, relaxation techniques, and exercise support recovery without pharmaceutical intervention.
Conclusion
Insomnia and addiction are deeply interconnected conditions that often reinforce one another, making recovery more complex. Because chronic sleeplessness is diagnosed alongside mental health or substance use concerns in many cases, integrated care is essential. Seeking professional treatment that addresses both issues increases the chances of long-term healing and improved quality of life.
FAQ
How are insomnia and addiction connected?
They are closely linked in a cycle where poor sleep can trigger substance use, and substance use worsens sleep.
What types of substances most commonly affect sleep?
Alcohol, stimulants, opioids, and sedatives are among the most disruptive to healthy sleep patterns.
Is it safe to use sleeping pills during addiction recovery?
Sleeping pills should be used with caution during recovery, as they may pose a risk for dependency.
Can insomnia increase the risk of relapse?
Yes, unmanaged insomnia can heighten stress and cravings, increasing relapse risk.
What are the best non-medication treatments for insomnia?
Cognitive Behavioral Therapy for Insomnia (CBT-I) and sleep hygiene practices are highly effective.
Should insomnia be treated before or after addressing addiction?
Both should be treated together through an integrated, dual diagnosis approach.
How can Calmerry help?
Calmerry offers accessible online therapy tailored to individuals struggling with both insomnia and addiction. Our licensed mental health professionals provide evidence-based approaches like CBT-I, helping clients improve sleep habits while addressing underlying emotional or behavioral patterns. With flexible plans and confidential support, Calmerry plays a supportive role in the recovery process by integrating care for co-occurring mental health challenges.
Robards, K. (2023, July 27). Understanding the relationship between sleep deprivation and addiction. Sleep Education. https://sleepeducation.org/understanding-relationship-between-sleep-deprivation-addiction/
International Classification of Sleep Disorders, 2nd Edition. (n.d.). Insomnia. https://aasm.org/resources/factsheets/insomnia.pdf
online therapy
live video session