Existential OCD: Understanding the Obsession with Life’s Deepest Questions
In this article
Most people, at some point in their lives, have engaged in existential – or philosophical – thinking. Questions like, “What is the meaning of life?” “What is my purpose?” or “Why do we exist?” are heavy, unanswerable questions.
But unlike the philosophical musing one might occasionally engage in, those with existential OCD find themselves imprisoned in an unending cycle of such profound questions.
This cycle can trigger overwhelming anxiety, existential dread, and consume their daily lives. While pondering life’s mysteries is a natural part of the human experience, these questions become a persistent and distressing whirlwind for some.
Understanding the complexities of existential OCD and seeking help can relieve the grip of these profound questions and anxieties.
What is existential OCD?
OCD, or obsessive-compulsive disorder, tends to bring up the stereotypical image of people needing to have things perfectly organized or those of people washing their hands frequently.
However, there are various subtypes of OCD that some people may not recognize. Existential OCD is one of them.
Existential OCD occurs when an individual is persistently troubled by existential or philosophical questions and concerns. This form of OCD revolves around intrusive and often distressing thoughts about meaning, life, death, reality, isolation, freedom, or the nature of the self. [1] International OCD Foundation. (2017, December 28). International OCD Foundation | To Be Or Not To Be, That Is The Obsession: Existential and Philosophical OCD. https://iocdf.org/to-be-or-not-to-be-that-is-the-obsession-existential-ocd/
People with existential OCD often experience intrusive questions such as, “What is real?” or “What happens after we die?”
Though many people explore philosophical questions, it can become a problem when these questions become debilitating, anxiety-provoking, and cause significant distress.
Existential OCD symptoms
The existential thoughts and intrusive questions that occur with this subtype of OCD cause significant distress. This distress distinguishes existential OCD from a typical midlife crisis or philosophical thinking.
Are these existential questions causing impairments in your daily life? Are you struggling to stop thinking about these questions and seeking constant reassurance?
If the answer is “yes,” it may indicate symptoms of existential OCD.
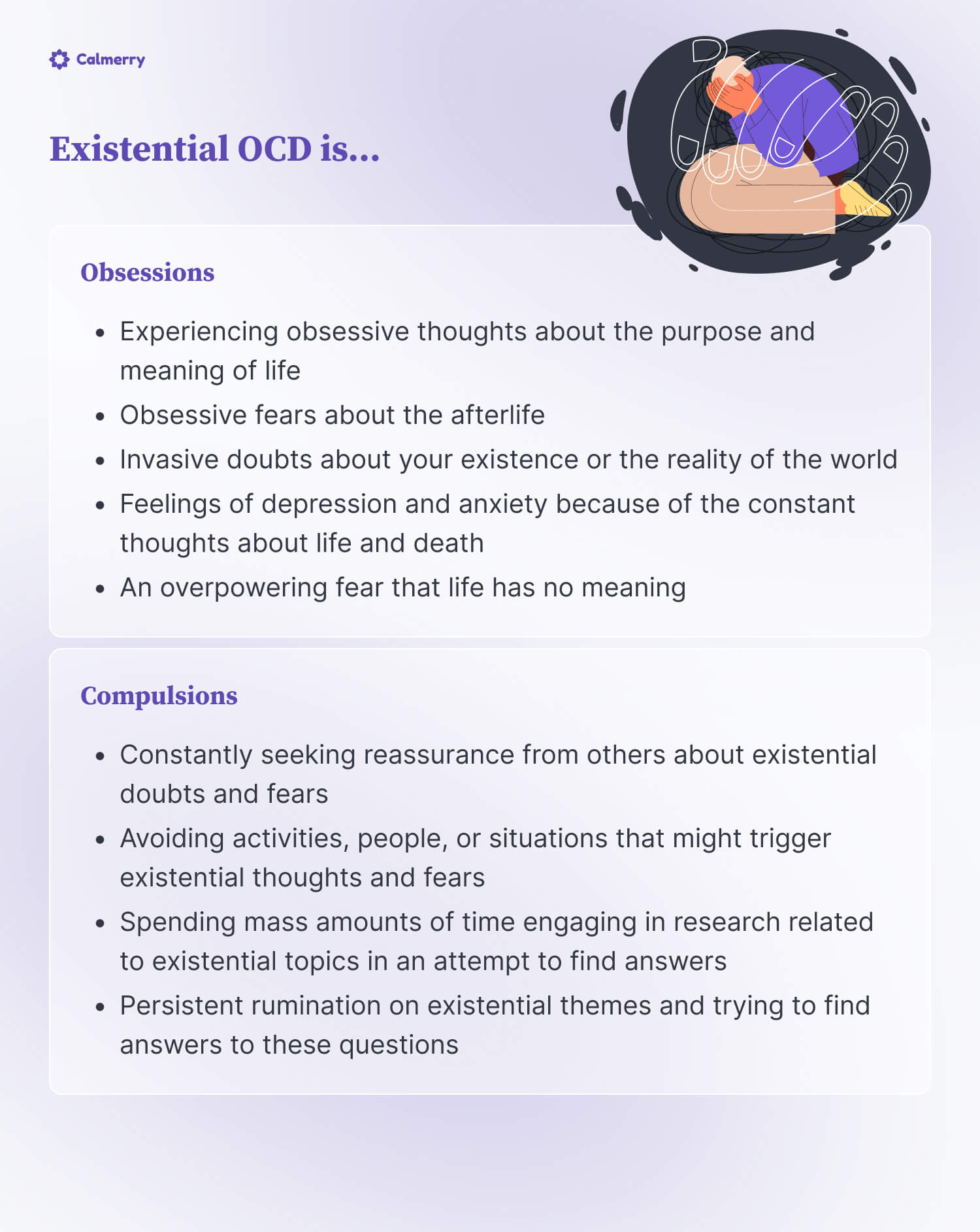
With any OCD, determining a diagnosis is related to a combination of obsessions and engaging in compulsive behaviors.
The obsessions and compulsions for existential OCD might include:
Obsessions
- Experiencing obsessive thoughts about the purpose and meaning of life
- Obsessive fears about the afterlife
- Invasive doubts about your existence or the reality of the world
- Feelings of depression and anxiety because of the constant thoughts about life and death
- An overpowering fear that life has no meaning
Compulsions
- Constantly seeking reassurance from others about existential doubts and fears
- Avoiding activities, people, or situations that might trigger existential thoughts and fears
- Spending mass amounts of time engaging in research related to existential topics in an attempt to find answers
- Persistent rumination on existential themes and trying to find answers to these questions
Because of these interfering obsessions and compulsions, those with existential OCD may experience impaired functioning in daily life, social isolation and strain in relationships, sleep disturbances, and difficulty concentrating.
Existential OCD examples
Some other examples of philosophical questions that are related to existential OCD are:
- Pervasive doubt: Continuous doubting of one’s existence, like often thinking, “Do I exist, or is this all a simulation?“
- Fear of non-existence: Intrusive thoughts about not existing after death and wondering, “What if there’s absolute nothingness after I die?“
- Perceptions of reality: Repeatedly questioning the nature of reality, thinking things like, “Is what I perceive real, or am I living in a dream?“
Like other forms of OCD, existential OCD might also involve compulsive behaviors to reduce the anxiety caused by these intrusive thoughts.
These behaviors could include extensive reading on philosophical topics, constantly seeking reassurance, or engaging in mental rituals like prayer or meditation to mitigate anxiety rather than for spiritual purposes.
Existential OCD vs. philosophical questioning
While many people – especially those who experience midlife or quarter-life crises – engage in philosophical thinking and have questions about the meaning of life and existence, there is a difference between general philosophical thoughts and existential OCD.
These philosophical questions about life and death can become OCD when they become obsessions that interfere with daily life. The questions, for those with existential OCD, are no longer a choice – they become involuntary and overwhelming.
General philosophical questions, on the other hand, do not cause distress or hinder your ability to focus on daily life.
If you have existential OCD, you may find tolerating the ambiguity and uncertainty of unanswered questions extremely difficult. This uncertainty can lead to feeling a pressing need for certainty and reassurance, which you try to alleviate your distress with compulsive behaviors like seeking constant validation.
Existential OCD and derealization
People with existential OCD may also experience derealization – a feeling of being detached from reality or that the world isn’t real. [2] APA Dictionary of Psychology. (n.d.). https://dictionary.apa.org/derealization
Existential OCD and derealization can occur because of the constant questioning about the purpose and meaning of life and the world.
Suppose you cannot come up with an appropriate or satisfactory answer. In that case, this can lead to disconnection from reality.
Can existential OCD cause depersonalization?
Similar to derealization, depersonalization occurs when one feels disconnected or detached from one’s physical body, thoughts, and emotions. [3] Depersonalization-derealization disorder – Symptoms and causes – Mayo Clinic. (2023, August 26). Mayo Clinic. https://www.mayoclinic.org/depersonalization-derealization-disorder/ You might start to question, “I don’t know who I am.”
When this occurs, it might feel like you are experiencing the sense of seeing yourself outside of your body – perceiving yourself in a dreamlike or unreal manner.
Research suggests that those with OCD may have a higher likelihood of experiencing derealization and depersonalization. It may be a way for the brain to protect you from overwhelming experiences and emotions. [4] Stoddard, G. (2023, May 22). Can OCD cause derealization? NOCD. https://www.treatmyocd.com/can-ocd-cause-derealization
– Veronica Silver, Therapist-turned mental health writer
The reasons that depersonalization/derealization may occur with OCD are not well understood. However, some theories discuss that it could be due to directing attention inward and focusing on internal processes or that sleep deficiencies may impair the systems that govern alertness and inhibition, resulting in feelings of disconnection from self and reality. [5] Soffer-Dudek N. (2023). Obsessive-compulsive symptoms and dissociative experiences: Suggested underlying mechanisms and implications for science and practice. Frontiers in psychology, 14, 1132800. https://doi.org/10.3389/fpsyg.2023.1132800
Regardless, existential OCD can cause depersonalization and is quite disturbing and distressing. So, getting treatment and managing the distress can help ease these symptoms.
Does existential OCD go away?
Like other forms of obsessive-compulsive disorder, existential OCD is often considered a chronic or long-lasting condition. [6] About OCD. (n.d.). Obsessive-Compulsive and Related Disorders. https://med.stanford.edu/ocd/about.html
But that does not mean the symptoms cannot be managed or decreased in intensity. With appropriate treatment and support, you can reduce the intensity, frequency, and impact of the symptoms and live a symptom-free life.
While it may not “go away” entirely for everyone, you can achieve substantial relief from symptoms and enjoy a high quality of life with the right interventions.
Treatment for existential OCD
If OCD is a chronic condition, how do you stop existential OCD? Not all is lost.
There are ways to treat and manage those intrusive obsessions and compulsions to live a happy and fulfilling life.
The treatment for existential OCD often includes a combination of therapy, medication, and self-help strategies.
Therapy
Therapy for OCD is one of the most effective forms of treatment.
Cognitive-behavior therapy, exposure and response prevention, and acceptance and commitment therapy have all effectively treated OCD.
Cognitive-behavioral therapy (CBT)
CBT focuses on identifying and challenging negative thoughts leading to unhelpful behaviors. With the help of a therapist, you can learn to challenge these thoughts and replace them with more helpful ones. [7] What is Cognitive Behavioral Therapy? (2017, July 31). https://www.apa.org. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
Exposure and response prevention (ERP)
This form of CBT is considered the gold standard for treating OCD. [8] Pittenger, C., Kelmendi, B., Bloch, M., Krystal, J. H., & Coric, V. (2005). Clinical treatment of obsessive compulsive disorder. Psychiatry (Edgmont (Pa. : Township)), 2(11), 34–43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2993523/
In ERP, those with existential OCD are gradually exposed to thoughts and ideas that scare them. They are then asked not to perform the compulsive behaviors that usually alleviate the distress.
As you work with a therapist to gradually go longer and longer without performing the compulsive behaviors, your anxiety reduces, and you can learn how to manage your emotions without responding.
– Veronica Silver, Therapist-turned mental health writer
Not performing compulsive behaviors might mean not asking others for reassurance but instead sitting with your doubts and letting them pass. [9] Fairfax, H. (2018, August 28). Mindfulness and Obsessive compulsive Disorder; Implications for Psychological Intervention. https://www.mentalhealthjournal.org/articles/mindfulness-and-obsessive-compulsive-disorder/ The more you practice this, the less distressing the experience.
Acceptance and commitment therapy (ACT)
It integrates acceptance and mindfulness strategies with behavior change.
When applied to OCD, ACT encourages individuals to accept their thoughts and feelings rather than fight against them while simultaneously committing to meaningful actions that enhance and enrich their lives.
For example, if you experience the existential thought of “do I exist?” With ACT, you learn to recognize the thought, accept the accompanying feelings without judgment, act in a way that aligns with values, and recognize the thought as merely a thought.
Medications
While there are no specific medications for treating OCD, some medicines can treat the anxiety and depression that typically accompany OCD.
The main medications used to treat OCD are anti-depressants such as SSRIs (selective serotonin reuptake inhibitors). [10] Pittenger, C., & Bloch, M. H. (2014). Pharmacological treatment of obsessive-compulsive disorder. The Psychiatric clinics of North America, 37(3), 375–391. https://doi.org/10.1016/j.psc.2014.05.006
These help increase and balance the serotonin in the brain.
Self-help strategies
In order to manage and reduce symptoms of existential OCD, it’s essential to implement and practice self-help strategies.
Some of the techniques that can help you manage existential depression, anxiety, and distress include:
Mindfulness practices
- Mindful breathing: When starting to experience distressing thoughts, engage in mindful breathing exercises. [11] Telloian, C. (2021, October 4). All about mindful breathing. Psych Central. https://psychcentral.com/health/mindful-breathing#benefits Mindful breathing combines deep breathing with mindfulness, focusing your attention solely on your breath to anchor your mind in the present moment.
- Observing thoughts: Practice observing your existential thoughts without judgment or engagement, allowing them to come and go like leaves floating down a stream.
Cognitive restructuring
- Thought records: Keep a thought record, noting triggering situations, the thoughts they induce, and alternative, more balanced thoughts.
Relaxation techniques
- Progressive muscle relaxation: Practice progressive muscle relaxation to manage physical symptoms of anxiety and stress.
- Guided imagery: Use guided imagery or visualization to create a mental space of calm and tranquility. Picture a place or event that causes you feelings of calm and relaxation. Practice picturing and holding that space in your mind, especially when experiencing anxiety or distress.
Journaling
- Expressive writing: Use journaling as an outlet for your thoughts, feelings, and experiences, creating a safe space to express existential fears without judgment. This writing can take 10-20 minutes to write freely about your emotions and distressing experiences. There is no right or wrong way to write as long as you can express yourself.
- Gratitude journaling: Keep a gratitude journal, noting aspects of life you’re thankful for to foster positive focus. We might not always feel so positive, especially when struggling with the anxiety of existential OCD, but practicing gratitude journaling can build up emotional resilience.
Seek support
- Join support groups: Consider joining a support group where you can share experiences and coping strategies with others who experience similar challenges. Having a space to feel seen and understood is helpful to reduce isolation.
- Consistent therapy: Ensure regular check-ins with your therapist to review and adapt strategies to manage existential OCD effectively.
On a final note
While these self-help techniques are great ways to continue progressing and managing symptoms, it is crucial to seek therapy to help you confront your distressing existential thoughts, obsessions, and compulsions.
Therapy can provide the tools and coping mechanisms to face these challenging experiences and improve your overall mental well-being.
For those who may not have access to in-person therapy, online therapy may be a viable option.
At Calmerry, you can be matched with an experienced mental health professional for your particular needs within 1 hour.
International OCD Foundation. (2017, December 28). International OCD Foundation | To Be Or Not To Be, That Is The Obsession: Existential and Philosophical OCD. https://iocdf.org/to-be-or-not-to-be-that-is-the-obsession-existential-ocd/
APA Dictionary of Psychology. (n.d.). https://dictionary.apa.org/derealization
Depersonalization-derealization disorder – Symptoms and causes – Mayo Clinic. (2023, August 26). Mayo Clinic. https://www.mayoclinic.org/depersonalization-derealization-disorder/
Stoddard, G. (2023, May 22). Can OCD cause derealization? NOCD. https://www.treatmyocd.com/can-ocd-cause-derealization
Soffer-Dudek N. (2023). Obsessive-compulsive symptoms and dissociative experiences: Suggested underlying mechanisms and implications for science and practice. Frontiers in psychology, 14, 1132800. https://doi.org/10.3389/fpsyg.2023.1132800
About OCD. (n.d.). Obsessive-Compulsive and Related Disorders. https://med.stanford.edu/ocd/about.html
What is Cognitive Behavioral Therapy? (2017, July 31). https://www.apa.org. https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
Pittenger, C., Kelmendi, B., Bloch, M., Krystal, J. H., & Coric, V. (2005). Clinical treatment of obsessive compulsive disorder. Psychiatry (Edgmont (Pa. : Township)), 2(11), 34–43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2993523/
Fairfax, H. (2018, August 28). Mindfulness and Obsessive compulsive Disorder; Implications for Psychological Intervention. https://www.mentalhealthjournal.org/articles/mindfulness-and-obsessive-compulsive-disorder/
Pittenger, C., & Bloch, M. H. (2014). Pharmacological treatment of obsessive-compulsive disorder. The Psychiatric clinics of North America, 37(3), 375–391. https://doi.org/10.1016/j.psc.2014.05.006
Telloian, C. (2021, October 4). All about mindful breathing. Psych Central. https://psychcentral.com/health/mindful-breathing#benefits
online therapy
live video session



