Does My Insurance Cover Online Therapy? How Do I Know?

In this article
As the healthcare landscape continues to evolve, insurance coverage policies are also changing. This is especially true for mental health services and online therapy, which have seen significant shifts in recent years.
Many people are exploring online therapy as a convenient and effective way to address their mental health needs. But understanding whether your insurance will cover online therapy can be confusing.
Insurance coverage for therapy varies widely depending on the provider, your location, and your specific plan. The recent changes due to the COVID-19 pandemic have added to the complexity.
So, does insurance pay for therapy?
Yes, insurance can pay for therapy. But it depends on your specific insurance plan and provider.
Many insurance plans include coverage for mental health services, often referred to as behavioral health benefits. But the extent of this coverage can vary widely. Some plans may cover only a certain number of sessions, while others might have stricter requirements about which types of therapy are covered.
Also, factors such as the type of therapy, the therapist’s qualifications, and whether the therapist is in-network or out-of-network can influence what is covered.
Is online therapy covered by insurance?
Many insurance providers expanded their mental health services to include telehealth. They respond to the increased demand for remote healthcare options.
While some of these expanded coverages remain, the specifics can vary greatly between different insurance providers and plans.
- Insurance plan coverage: many insurance plans, including those offered by employers and individual/family plans through the healthcare marketplace, now cover some form of online or telehealth services. But the specifics of what is covered can vary greatly between plans.
- Type of online therapy: most insurance plans that cover telehealth will reimburse for live video sessions with a therapist licensed in your state. Some may also cover asynchronous therapy via messaging or other means of communication.
- Provider network: insurance companies typically have a network of approved telehealth providers. Coverage and reimbursement rates are highest when you use an in-network provider.
- Deductibles and co-pays: even if online therapy sessions are covered, you’ll likely need to pay any applicable deductibles and co-payments required by your plan.
- State laws: some states have laws that mandate insurance coverage for telehealth services under certain circumstances.
The best way to determine if your specific online therapy will be covered is to check with your insurance provider directly. Request details on their telehealth policies, approved provider lists, co-pay requirements, and any limits on the number of covered virtual sessions.
Many insurers are increasing telehealth coverage, but verifying ahead of time is advisable.
Examples of insurance providers covering online therapy
Several major insurance providers cover online therapy, including:
- Aetna
- Blue Cross Blue Shield
- UnitedHealthcare
- Medicare
- Medicaid
How do I know if my insurance covers therapy?
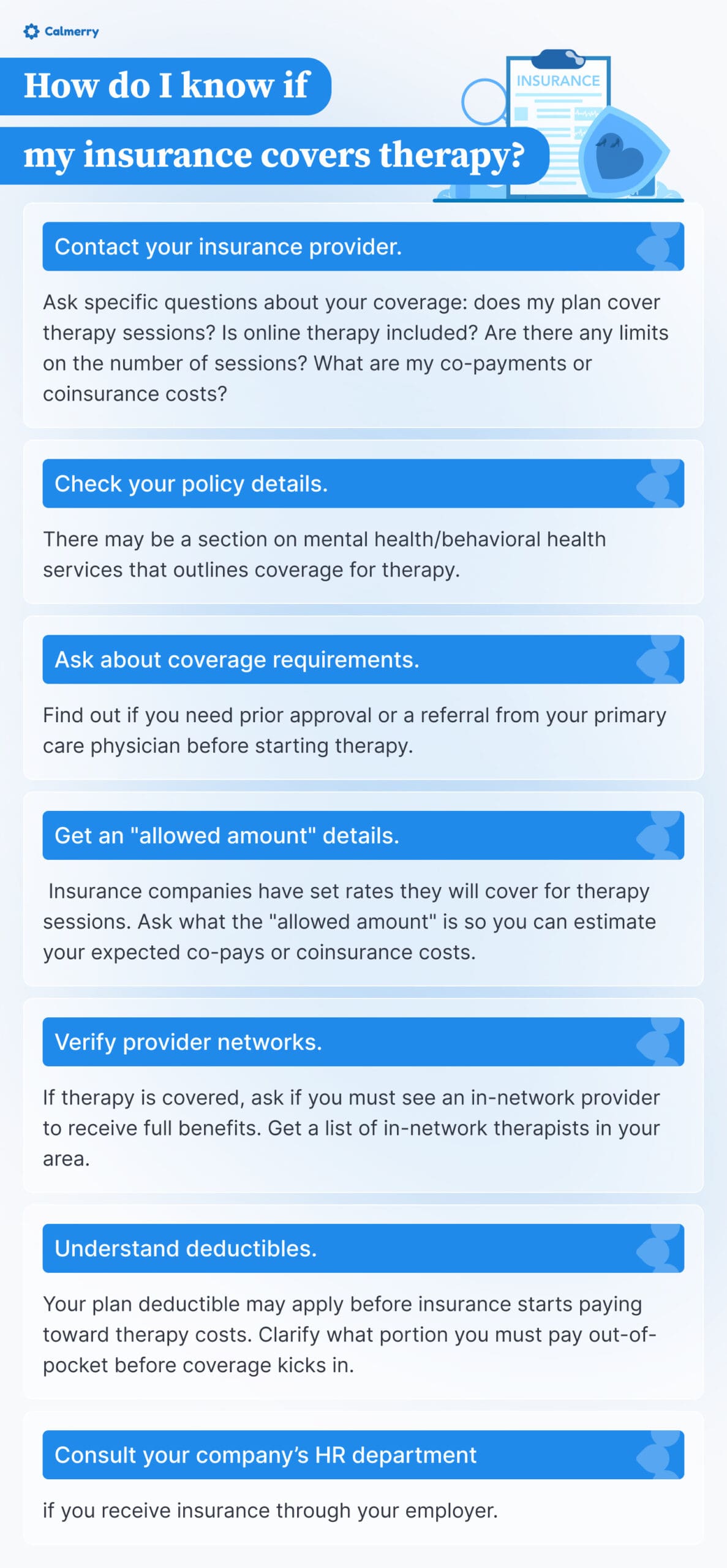
- Check your policy details. Look through the paperwork or online information for your specific insurance plan. There may be a section on mental health/behavioral health services that outlines coverage for therapy.
- Contact your insurance provider. Call the customer service number on your insurance card. A representative can look up your plan details and let you know if outpatient therapy sessions are a covered benefit and what your costs would be. Ask specific questions about your coverage, such as: does my plan cover therapy sessions? Is online therapy included? Are there any limits on the number of sessions? What are my co-payments or coinsurance costs?
- Ask about coverage requirements. Find out if you need prior approval or a referral from your primary care physician before starting therapy. Also, ask if there are any limits on the number of covered sessions.
- Get an “allowed amount” details. Insurance companies have set rates they will cover for therapy sessions. Ask what the “allowed amount” is so you can estimate your expected co-pays or coinsurance costs.
- Verify provider networks. If therapy is covered, ask if you must see an in-network provider to receive full benefits. Get a list of in-network therapists in your area.
- Understand deductibles. Your plan deductible may apply before insurance starts paying toward therapy costs. Clarify what portion you must pay out-of-pocket before coverage kicks in.
- Consult your company’s HR department. If you receive insurance through your employer, your HR department can provide detailed information about your coverage options and help you navigate any changes or updates to your plan. They can also assist in finding in-network providers and understanding the specifics of your workplace mental health benefits.
How many therapy sessions does insurance cover?
There’s no one-size-fits-all answer for how many therapy sessions insurance will cover. The number of covered sessions can vary significantly depending on:
- Your specific insurance plan
- Whether you have met your deductible
- If you need pre-approval or have coverage limits
- The reason/diagnosis for pursuing therapy
However, here are some typical situations that may apply:
- Many insurance plans cover 20-30 outpatient therapy sessions per year.
- For specific mental health diagnoses like depression or anxiety, higher session limits like 40-60 visits may be covered.
- Some comprehensive plans cover unlimited sessions deemed medically necessary.
- Health Maintenance Organization (HMO) plans often require pre-approval after a set number of sessions.
- High-deductible plans may not cover therapy costs until the deductible is met.
The best way to get an accurate answer is to contact your insurance provider directly. Request the specific details about outpatient mental health coverage, including:
- Session limits or maximums
- Required co-pays or coinsurance
- Deductible requirements
- Specifications for in-network vs. out-of-network providers
Having this information upfront can help you plan and budget for the expected therapy costs. Coverage can vary substantially across different insurance plans.
Calmerry – affordable online therapy
We provided an exhaustive answer on whether online therapy on Calmerry is covered by insurance.
Please ask your provider if they can cover your therapy costs – we can provide a receipt for reimbursement.
If your insurance plan doesn’t cover online therapy, or if you don’t have insurance, Calmerry remains an accessible option for quality mental health care at a reduced cost. Our mission is to make therapy accessible to everyone.
You will get help from licensed, trained, and experienced therapists online, but at a reduced cost.
Our cost-saving measures
- Promo codes for the first month: apply promo codes at checkout to save up to 30% on your first month.
- Financial aid: after your first month, you can receive up to 30% off for the next three months.
- Free self-help tools in the app: our app offers a range of tools designed to support your mental well-being
The Calmerry app is free on both Android and iOS platforms. Simply register, complete a survey, skip choosing a plan, and access your account to use these tools.
online therapy
live video session