What Is “Cyclical Depression?” Types, symptoms, and Treatment

In this article
Cyclical depression is a form of depression in which symptoms follow distinct patterns.
Cyclical depression is not a clinical diagnosis but an umbrella term that includes several subtypes, including seasonal affective disorder (SAD) and cyclothymia.
This article will outline the types, symptoms, and treatment of cyclical depression.
How does cyclical depression differ from other forms of depression?
Cyclical depression can be difficult to distinguish from other forms of depression since it shares many of the same symptoms.
However, while the symptoms of other depressive disorders follow no identifiable pattern, the symptoms of cyclical depression occur at regular intervals.
These intervals may be seasonal, tied to a woman’s menstrual cycle, or alternate with periods of feeling more upbeat and energetic than usual.
Also, the symptoms of cyclical depression may be less numerous or severe than those of other forms of depression.
Types of cyclical depression
There are several distinct types of cyclical depression, each with unique triggers and symptom patterns.
Although all types can be treated with medication and/or psychotherapy, some types of cyclical depression also respond to alternative therapies such as Vitamin D supplements or oral contraceptives.
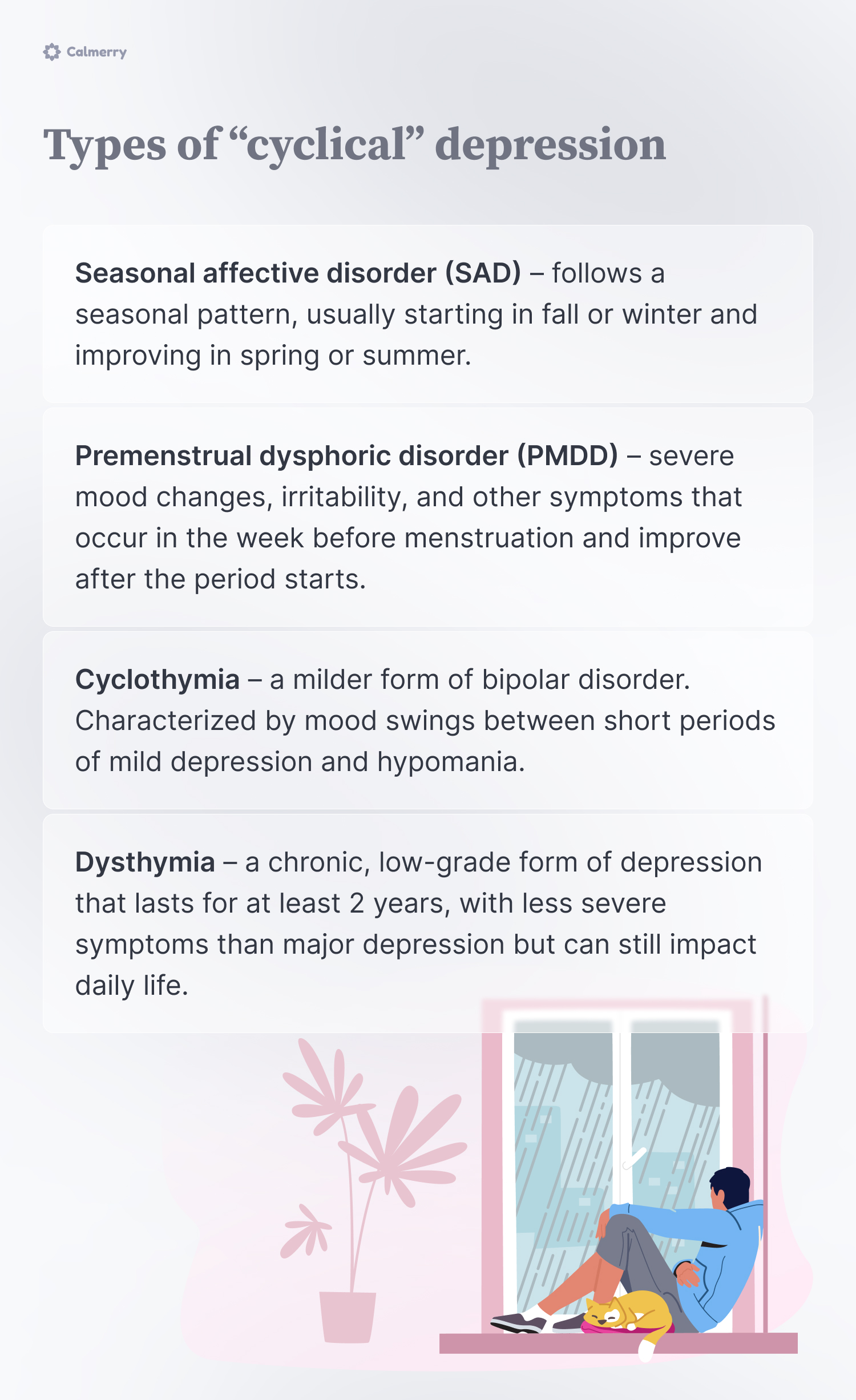
Seasonal affective disorder (SAD)
The symptoms of seasonal affective disorder fluctuate with the seasons.
For most people, symptoms get worse during the fall and winter months. However, some experience worsening mood during the spring and summer.
The cause of SAD is unknown but is thought to be related to hormonal changes triggered by sunlight. Research indicates that people with SAD have atypical levels of melatonin, a hormone involved in sleep regulation. [1] Seasonal affective disorder. (n.d.). National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/publications/seasonal-affective-disorder
Other studies have shown lower levels of serotonin, a brain chemical that regulates mood, in people suffering from SAD.
Here are some other symptoms of SAD:
- Seasonal changes in energy level
- Seasonal changes in sleep patterns
- Difficulty concentrating
- Restlessness
- Social withdrawal
- Feeling sad, hopeless, or worthless
Treatment options specific to SAD include light therapy and vitamin D supplements.
Light therapy uses artificial light to regulate your boy’s natural circadian (sleep) rhythms. Vitamin D is believed to promote serotonin activity, helping with mood regulation.
Your healthcare provider may also recommend lifestyle changes to help with SAD, including spending time outdoors.
Premenstrual dysphoric disorder (PMDD)
Premenstrual dysphoric disorder, or PMDD, is characterized by a range of emotional, cognitive, and physical symptoms coinciding with the phases of the female menstrual cycle.
Typically, these symptoms start 1 to 2 weeks before the start of menstruation and end when a woman gets her period, but everyone is different.
PMDD is different from premenstrual syndrome, or PMS, in that its symptoms are more severe and debilitating.
Here are some of the most common symptoms of PMDD:
- Irritability
- Mood swings
- Anxiety
- Depressed mood
- Low energy
- Changes in appetite or sleep
- Feeling overwhelmed
- Difficulty focusing
- Breast tenderness
- Headache
- Bloating
Because PMDD is thought to be associated with hormonal fluctuations, it is sometimes treated with oral contraceptives, aka “the pill.” These medicines help to regulate the female reproductive hormones estrogen and progesterone.
Cyclothymia
In cyclothymia, depressive symptoms alternate with periods of hypomania. Hypomania is characterized by elevated or irritable mood, increased energy, and decreased need for sleep.
Because of this, cyclothymia is thought to be a less severe form of bipolar disorder. Unlike the manic episodes of bipolar disorder, hypomania generally does not cause significant distress or impairment.
Nonetheless, it is important for people with cyclothymia to seek treatment, since hypomania can be a precursor to mania.
Symptoms of cyclothymia include:
- Talking more than usual
- Feeling more confident than usual
- Increased motivation
- Increase in risky behavior
- Irritability
- Sadness
- Low energy
- Loss of interest in activities
- Social withdrawal
- Hopelessness
Dysthymia
Unlike other types of cyclical depression, dysthymia is characterized by long-standing, unremitting depressive symptoms. For this reason, dysthymia is sometimes referred to as persistent depressive disorder or chronic depression.
The symptoms of dysthymia are typically less severe than those of major depressive disorder (MDD). However, people with MDD can experience periods of remission from depression, while the symptoms of dysthymia last for 2 years or longer.
Symptoms of dysthymia include:
- Chronic fatigue
- Insomnia
- Poor concentration
- Inability to experience joy
- Lack of interest in activities
- Hopelessness
Dysthymia should be distinguished from recurrent or refractory depression, both of which are also sometimes referred to as “chronic”:
- Recurrent depression is characterized by repeated depressive episodes alternating with periods of remission.
- Refractory depression is depression that doesn’t respond to standard treatments such as medication and psychotherapy.
Is it normal to have cycles of depression?
Everyone has emotional ups and downs. For those with cyclical depression, however, the downs are more severe and have a bigger impact on daily life.
Someone who is having a low day can typically still drag themselves to work, get together with friends, or feel optimistic about tomorrow. Someone with cyclical depression, on the other hand, usually finds it hard to function in one or more areas of life.
The World Health Organization (WHO) estimates that 280 million people suffer from some form of depression. [2] World Health Organization: WHO & World Health Organization: WHO. (2023, March 31). Depressive disorder (depression). https://www.who.int/news-room/fact-sheets/detail/depression In fact, depression is one of the most common mental health conditions worldwide.
While cycles of depression may seem “normal” in this context, it doesn’t mean that depression isn’t a serious condition that can get worse if left untreated.
Unfortunately, approximately 60% of people with depression do not seek treatment. [3] Chand, S. P., & Arif, H. (2023, July 17). Depression. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK430847/
Factors that may contribute to the development of cyclical depression
There is no one cause of cyclical depression. However, several factors make you more likely to develop SAD, PMDD, cyclothymia, or dysthymia.
These include:
History of trauma
Trauma impacts the areas of the brain responsible for emotion regulation and stress response. This can increase your vulnerability to cyclical depression.
Trauma can also lead to negative beliefs about yourself, the world, and other people. These beliefs often create a sense of hopelessness and disconnection from others, preventing you from reaching out for support or treatment.
Family history of depression
Research indicates that there is a genetic component to depression. [4] Major Depression and Genetics. (n.d.). Genetics of Brain Function. https://med.stanford.edu/depression-genetics/mddandgenes.html If an immediate family member has depression, you could be 2-3 times more likely to develop it yourself.
However, no specific genes have been identified as causing depression, and just because you have a family history does not mean you will become depressed yourself.
Where you live (SAD)
People who live in areas farther from the equator are more likely to develop SAD than those who live closer to it. These regions have long, dark winters, which can disrupt the body’s circadian rhythms and lead to low energy and depressed mood.
Your gender at birth (PMDD)
Since the symptoms of PMDD coincide with different phases of the menstrual cycle, only menstruating people can be diagnosed with PMDD.
However, hormonal changes during pregnancy, post-childbirth, and in the years leading up to menopause can also cause or exacerbate symptoms of depression.
These hormonal fluctuations are believed to be the reason that females are more at risk for all forms of depression.
Stress
When we are stressed, our bodies release hormones like cortisol and adrenaline. In the short term, these hormones help us respond to the crisis. However, over time, stress can lead to changes in brain chemistry and structure.
Moreover, stress often correlates with poor sleep, unhealthy eating habits, and substance use, all of which can exacerbate symptoms of depression.
– Lindsay Renner Schwartz, Licensed Clinical Social Worker (LICSW)
How long does cyclical depression last?
The length of depression varies from person to person and depends on multiple factors, including whether treatment is initiated and the presence of various life stressors.
That said, to be diagnosed with dysthymia, you must have consistent symptoms for at least 2 years.
The depressive episodes of PMDD or cyclothymia are typically shorter, lasting 2 weeks or less.
Finally, the symptoms of SAD may last for an entire season.
Treatment options
The good news is that all forms of depression, including cyclical depression, are treatable.
The first step is to meet with a licensed mental health provider to talk about your symptoms, history, and the depression therapy that might work best for you.
Here are a few of the treatments available for cyclical depression:
Psychotherapy
Also known as talk therapy, psychotherapy involves meeting one-on-one with a therapist or counselor.
There are many different types of psychotherapy for depression.
For example, cognitive-behavioral therapy focuses on negative thought patterns and behaviors that may be contributing to your depressive symptoms.
Psychodynamic therapy examines the role of early life events and relationships.
And dialectical behavioral therapy involves systematically learning and practicing skills for better emotion regulation and distress tolerance.
Medication
Often used in conjunction with psychotherapy, antidepressant medications help to correct the biochemical imbalances associated with cyclical depression.
Selective serotonin reuptake inhibitors (SSRIs), such as Prozac and Zoloft, are often the first line of treatment for PMDD, SAD, and dysthymia.
Cyclothymia is more likely to be treated with mood-stabilizing medications, as antidepressants can exacerbate hypomanic symptoms. You may need to try a few different medications to find what works best for you.
Lifestyle changes
Some lifestyle changes can alleviate symptoms of cyclical depression.
For example, exercise is a powerful mood enhancer, regardless of the type and intensity.
Stress-reduction techniques such as mindfulness meditation may also be helpful, as they can strengthen your social connections and limit your consumption of alcohol and other drugs.
Coping strategies
In addition to the above, you can use coping strategies to manage symptoms of cyclical depression.
If your depressive cycles are predictable, such as with PMDD and SAD, you may want to plan to make self-care a priority during the more challenging weeks/months.
Self-care looks different for everyone but often includes maintaining a regular sleep schedule, eating a balanced diet, and engaging in relaxing and/or enjoyable activities.
Here are some other coping strategies for cyclical depression:
Social support
When you are depressed, your instinct may be to self-isolate. However, research indicates that social support plays a crucial role in reducing the symptoms of depression.
For example, a study of university students found that those who had more social support were less likely to be depressed, even when reporting high levels of stress. [5] Wang, X., Cai, L., Qian, J., & Peng, J. (2014). Social support moderates stress effects on depression. International Journal of Mental Health Systems, 8(1). https://doi.org/10.1186/1752-4458-8-41
Make a list of people you can contact when you are feeling depressed. Ask friends and family to check in on you if they haven’t heard from you for a while.
Schedule social engagements for times when your symptoms tend to worsen. It doesn’t have to be elaborate – for example, invite a friend for takeout and a movie.
Spending time in nature
Exposure to natural environments like parks, gardens, and beaches can help alleviate depression, even if your symptoms do not follow a seasonal pattern.
A 2015 study found that people who walked in nature for 90 minutes showed decreased activity in the areas of the brain associated with depression. [6] Zarr, R., & Chan, W. (2023, December 8). Nature: A Key Ingredient for Mental Health. The Pew Charitable Trusts. https://www.pewtrusts.org/en/trend/archive/fall-2023/nature-a-key-ingredient-for-mental-health
If you live in an urban environment without a lot of green spaces, try creating an indoor oasis. Research indicates that spending time among houseplants can reduce stress, improve focus, and boost overall life satisfaction. [7] Haupt, A. (2023, March 2). Your houseplants have some powerful health benefits. TIME. https://time.com/6258638/indoor-plants-health-benefits/
Therapeutic journaling
Journaling is another helpful tool for managing cyclical depression. Writing down your thoughts and feelings can decrease rumination and help you identify patterns of symptoms.
You don’t have to be a wordsmith to benefit from this coping strategy. Try a mood journal with a pre-printed symptom checklist or an art journal that allows you to draw or collage how you are feeling.
– Lindsay Renner Schwartz, Licensed Clinical Social Worker (LICSW)
Short on time? Use a gratitude journal to jot down 2-3 positive things in your life. This simple exercise takes less than a minute and has been shown to decrease stress and improve mood. [8] Fekete, E. M., & Deichert, N. T. (2022). A brief gratitude writing intervention decreased stress and negative affect during the COVID-19 pandemic. Journal of Happiness Studies, 23(6), 2427–2448. https://doi.org/10.1007/s10902-022-00505-6
One of the most challenging things about depression is that it robs you of the energy and motivation to do the things that might help you to feel better. Thus, self-care during a depressive episode often requires walking a fine line between cutting yourself some slack and pushing yourself to engage in mood-boosting activities.
You don’t have to manage cyclical depression on your own! A professional therapist can provide individualized recommendations based on your symptoms, history, and lifestyle.
A word from Calmerry
At Calmerry, we understand the unique challenges that come with cyclical depression.
Our team of licensed and experienced therapists is well-equipped to help you navigate the ups and downs of depression.
They specialize in various treatment approaches, including cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and interpersonal therapy (IPT), which have been shown to be effective in managing cyclical depression.
They can work with you to develop a personalized treatment plan that addresses your specific needs and goals.
We know that finding the right therapist is crucial for a successful therapy experience. That’s why we offer a unique therapist-matching service.
Simply fill out our brief questionnaire – and within 1 hour, we’ll match you with a therapist who aligns with your preferences and needs.
Seasonal affective disorder. (n.d.). National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/publications/seasonal-affective-disorder
World Health Organization: WHO & World Health Organization: WHO. (2023, March 31). Depressive disorder (depression). https://www.who.int/news-room/fact-sheets/detail/depression
Chand, S. P., & Arif, H. (2023, July 17). Depression. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK430847/
Major Depression and Genetics. (n.d.). Genetics of Brain Function. https://med.stanford.edu/depression-genetics/mddandgenes.html
Wang, X., Cai, L., Qian, J., & Peng, J. (2014). Social support moderates stress effects on depression. International Journal of Mental Health Systems, 8(1). https://doi.org/10.1186/1752-4458-8-41
Zarr, R., & Chan, W. (2023, December 8). Nature: A Key Ingredient for Mental Health. The Pew Charitable Trusts. https://www.pewtrusts.org/en/trend/archive/fall-2023/nature-a-key-ingredient-for-mental-health
Haupt, A. (2023, March 2). Your houseplants have some powerful health benefits. TIME. https://time.com/6258638/indoor-plants-health-benefits/
Fekete, E. M., & Deichert, N. T. (2022). A brief gratitude writing intervention decreased stress and negative affect during the COVID-19 pandemic. Journal of Happiness Studies, 23(6), 2427–2448. https://doi.org/10.1007/s10902-022-00505-6
online therapy
live video session