Borderline Personality Disorder: What You Need to Know

In this article
Relationships, emotions, likes and dislikes, behaviors, and self-image change abruptly, like the weather, reacting to the slightest changes in the environment. Frequent mood swings, seeing things in extremes, impulsiveness, intense fear of rejection and abandonment, difficulty managing emotions, “all good or all bad” — for a person with borderline personality disorder, every aspect of life may feel unstable.
Borderline personality disorder (BPD) is widely discussed today also in terms of one the most stigmatized conditions. It prevents people from getting the effective treatment they need. Often, they try to handle the symptoms alone and deal with the preconceptions of others.
What is borderline personality disorder?
Borderline personality disorder is also known as emotionally unstable personality disorder (EUPD). This disorder is marked by a dysfunctional regulation of emotions.

This condition is characterized by:
- Impulsivity
- Emotional instability
- Distorted self-image
- High anxiety levels
- Intense anger, irritability
- A feeling of emptiness
- A pattern of unstable relationships
- Dissociative symptoms
- Feelings of shame and guilt
- Sensitiveness to criticism and failure
- Seeing the world in white and black extremes
- Self-destructive behavior, etc.
Mostly, BPD is diagnosed during adolescence or early adulthood.
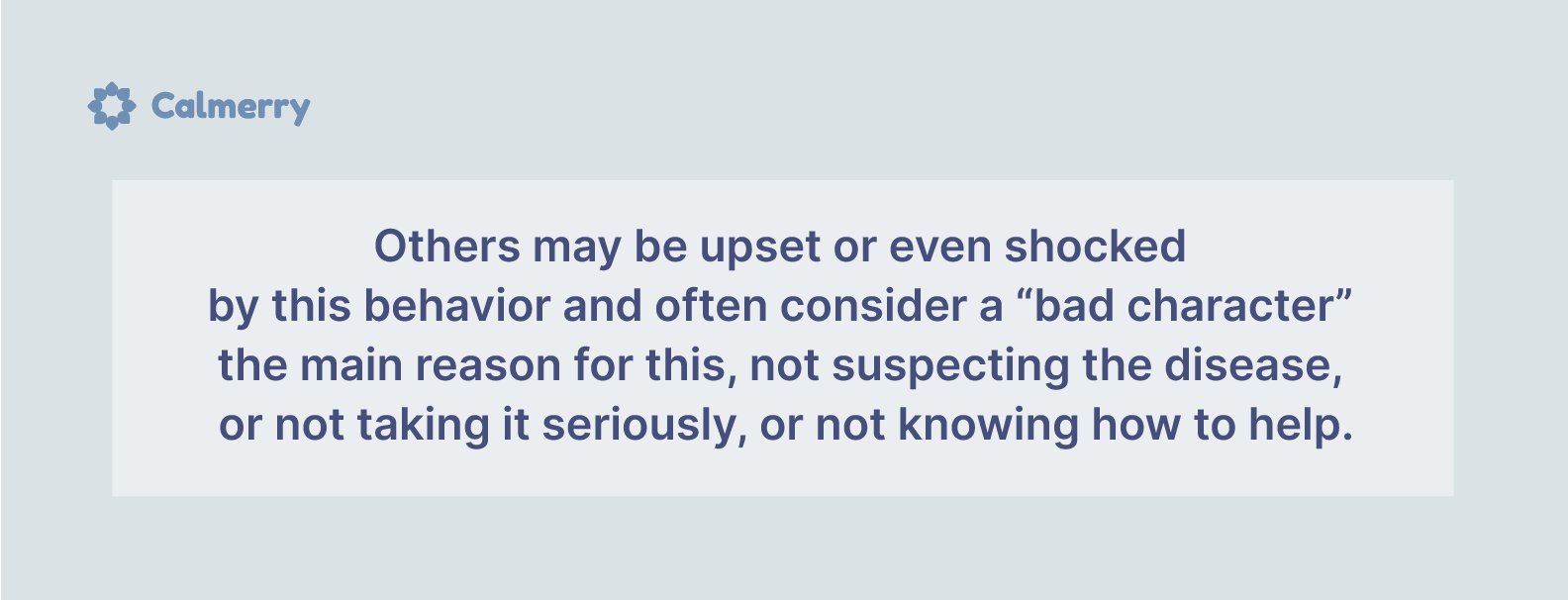
When trying to share their worst experiences with their close circle of people and discuss what’s going on with them, it’s common for people with BPD to hear something like:
- “That’s just how you react to stuff around you.”
- “It’s just your character.”
- “You’re making this up, you just want to attract attention!”, etc.
Lack of support aggravates mental health problems in people with borderline personality disorder and may make their lives unbearable. All their experiences feel overwhelming. So they need full understanding and support.
With the appropriate help of healthcare professionals, self-care, emotional support, and the right treatment, it’s possible to live a fulfilling life.
Why is borderline personality disorder called “borderline”?
Earlier, mental illnesses were classified into “psychoses” and “neuroses” groups. And BPD has been described as a “mild form of schizophrenia,” being at the “border” of psychosis and neurosis.
As a personality disorder diagnosis, BPD was recognized only in 1980. Today, many clinicians agree that the term “borderline” is controversial, stigmatizing, has no descriptive value, and should be changed.
Research is currently focused on problems with emotional regulation, thinking and behavioral patterns, and relationship and interpersonal problems as core aspects of borderline personality disorder.
Causes of borderline personality disorder
The exact causes of borderline personality disorder are yet to be discovered.
There are some potential factors that may play a role in the development of this disorder:
- Early childhood stressful experiences, adversity
- Trauma
- History of emotional, physical, or sexual abuse
- Separation or loss of a caregiver
- Emotional detachment in the parent-child relationships
- Neglect of a child’s opinions and feelings
- PTSD
- Genetic predisposition
- Structural and functional changes in the brain and neuroregulatory systems

However, not everyone who had these experiences will have BPD. And it’s more likely that a combination of factors is responsible for the development of this disorder rather than a single reason.
When does BPD develop?
Borderline Personality Disorder (BPD) typically develops during adolescence or early adulthood. Its roots can often be traced back to earlier in life, influenced by a combination of genetic, environmental, and social factors.
What is a BPD favorite person?
In the context of borderline personality disorder, a “favorite person” (FP) is a significant individual in the life of someone with BPD. This person becomes the focal point of the individual’s emotional world. This often leads to intense and sometimes turbulent dynamics.
The individual with BPD forms a very strong emotional bond with their FP, often experiencing extreme dependence on their presence and approval. The FP becomes the primary source of validation, support, and emotional stability.
The relationship may swing between idealizing the FP, viewing them as perfect and essential, and devaluing them, seeing them as flawed and disappointing. These shifts can occur rapidly and unpredictably, often triggered by perceived slights or fears of abandonment.
There is a constant fear of being abandoned or rejected by the FP with anxiety and efforts to keep the FP close. And the FP might feel they are walking on eggshells to avoid causing distress, which can be exhausting and unsustainable
Borderline personality disorder symptoms & signs
Borderline personality disorder isn’t easily diagnosed. Every person is different, and their experience of BPD differs, too. Not all people with BPD have all symptoms below, and experiencing some of them doesn’t mean having BPD.
To receive a diagnosis, a person must meet 5 out of 9 DSM-5 diagnostic criteria:
1. Intense worry about real or imagined abandonment
People with BPD can be alone but don’t tolerate abandonment — both imagined and real — and are desperate to avoid it. The thought of their favorite person (not necessarily a romantic partner) abandoning or rejecting them is unbearable.
Also, it’s extremely difficult for people with BPD to leave someone. So it’s common for them to stay in an unhealthy or abusive relationship, although they would like to be in healthy ones.
They may experience anger outbursts, panic, and feel helpless when faced with real time-limited separation or changes in daily life plans.
For example, should a loved one not answer the call, be late for a meeting, or not put a heart emoji in a goodnight message, a person with BPD can plunge into self-devaluation (“I’m bad and not worthy to be with them, my partner doesn’t love me, our relationship is a lie.”) or show aggression towards the “offender” (“How dare you?!”).
2. Unstable interpersonal relationships and seeing the world in extremes
Due to frequent mood swings and unexpected changes in attitudes either to oneself or to a partner, a relationship with the BPD person turns into a rollercoaster. They may idealize their partner and then devalue them — they now can be the best, but if a partner says something “wrong,” they hate them. Sometimes, this happens almost simultaneously.
The perception of the world only in black and white, when there are two extremes, two sides — all good or all bad — creates more challenges in life.
3. Distorted self-image and a weak sense of self
People with BPD have a very vague sense of self and may feel a differing self-image often. There is a constant balancing on the border — “I am nothing, and then a genius.” Their opinion about themselves directly depends on how others perceive them. Often, these opinions are incorrect since they are based on the last impression they left on someone.
People with borderline personality disorder can “adopt” habits, behavioral patterns, and interests of their favorite person whom they perceive as their “mirror reflection.” They don’t know who they are and what they need. Today it may be one thing, tomorrow is another.
Therefore, they constantly rush, change, and adjust. They change their values, goals, career, partners, religion, sexual orientation, etc. Often, such people are not taken seriously and suffer from their internal instability. All these contribute to the development of depression, anxiety, and stress-related disorders.
4. Impulsive, self-damaging behavior in at least two areas
A person with BPD tends to engage in risky behaviors and have reckless decisions and intense emotional reactions that lead to accidents.
Their impulsivity may easily lead them into dangerous situations, especially when distressed:
- Impulsive money spending
- Reckless driving
- Binge eating
- Sexual promiscuity
- Substance abuse
- Law violation, etc.
5. Self-harm and suicidal behavior
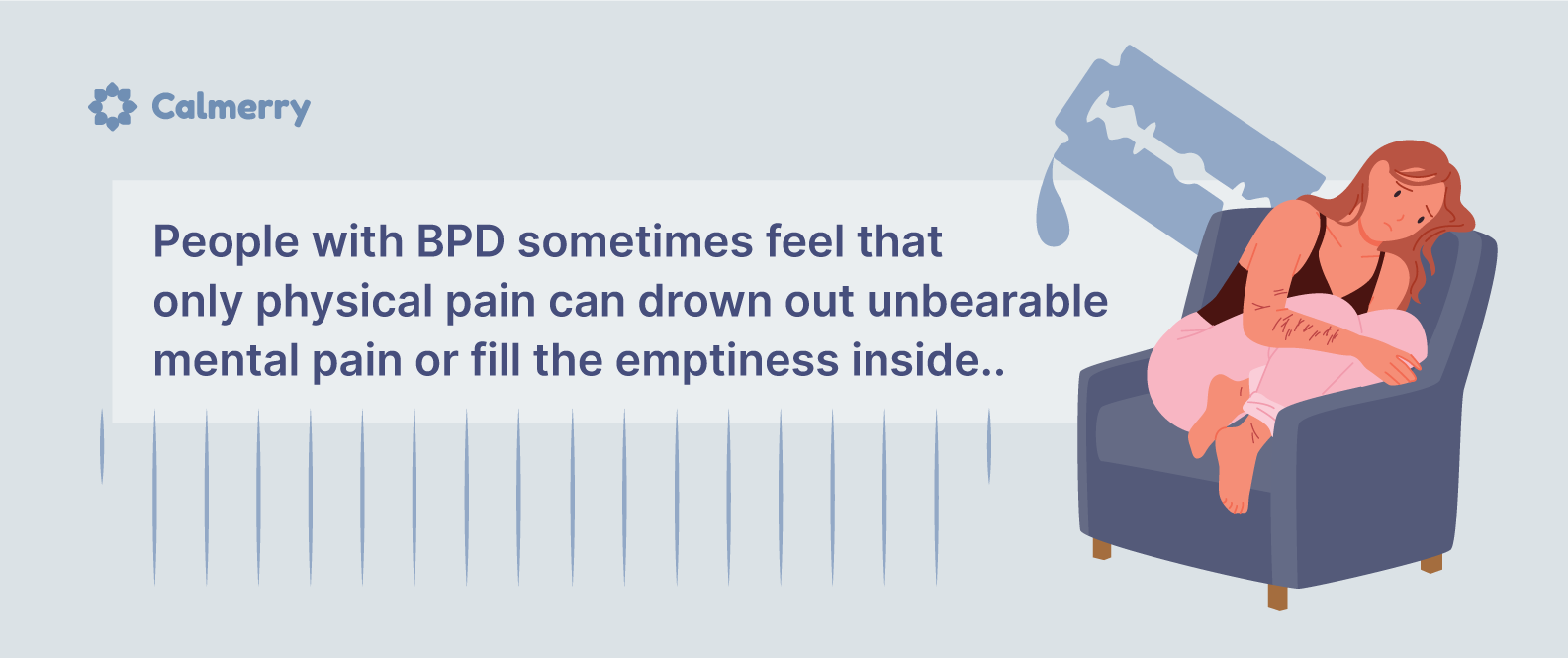
Self-harm in people with BPD is common. Through self-mutilative acts, a person tries to feel that they are alive and exist.
Also, one of the most important diagnostic signs of BPD is recurrent suicidal tendencies. According to statistics, about 10% of people with BPD die as a result of suicide.
People in crisis need help right away. If you experience suicidal thinking or behavior, call 911 or your local emergency number.
6. Reactivity of mood and emotional instability
- People with BPD experience extreme mood swings
- Have trouble dealing with intense emotions
- Tend to suppress their emotions
- Have difficulty developing stable relationships with others or establishing healthy boundaries
- Often act in impulsive and potentially self-damaging ways
Usually, their emotional responses are not proportional to the situation.
They can often find themselves in and out of crisis and intense emotional states that they just cannot control.
People with BPD react more intensely to emotional situations because of the sudden and unpredictable nature of their emotional reactions. They can be sweet one moment and then lash out in anger for a few hours.
This inconsistency in the reaction can leave others wondering what caused this sudden shift, take a toll on their relationships with a BPD person, and affect their mental health.
Also, sufferers can become extremely frustrated because they cannot communicate their feelings effectively or regulate their emotions.
7. Chronic feeling of emptiness
They often suffer in silence, make decisions in secrecy, abandon social relationships, and feel an emptiness. Often, it’s described as a feeling that a person is missing something inside and has a strong desire, a thirst to fill it.
This feeling of emptiness is sharp, constantly present, and not familiar to many people.
People with BPD often engage in maladaptive behavior or self-harm to fill the void. For example, they try to self-medicate the feeling of emptiness with alcohol.
8. Intense anger or poor anger management
They may try to control situations with threats, acting impulsively or, often, aggressively. They may not listen to what others say, which leads to escalating arguments.
Additionally, speaking up may trigger their distress or hurt their feelings, leading them to act even more aggressively.
It’s difficult for them to control their anger, and after the displays of temper, they can experience:
- Shame
- Guilt
- Frustration
- Self-pity
- Detachment
- Rumination
It’s a vicious cycle that intensifies anger and increases its duration. Eventually, they end up often acting out in ways that are destructive to themselves and others.
Also, recurrent physical fights and self-directed anger are some of the displays of aggressiveness.
9. Paranoid ideation and severe dissociative symptoms
When these people are under stress, they may have short episodes of paranoia, psychotic-like symptoms (such as hallucinations), or dissociation. They can “block” intense painful emotions.
Feeling of the unreality of what is happening (derealization) or a feeling of distance from your body or thoughts (depersonalization) are also common borderline personality disorder symptoms.
People with BPD can “forget” about themselves, existing in other, imaginary worlds. They are often obsessed with books, movies, and various fandoms and associate themselves with some characters.
How is borderline personality disorder diagnosed?
Considering all that has been said, don’t worry if you recognize yourself in some of these symptoms. This doesn’t automatically mean that you have BPD.
But if you suspect that you or your loved one has borderline personality disorder, and if the symptoms are devastating for both you and the people around you, see a mental health professional.
You can take a number of tests on the Internet and find all the symptoms in yourself. However, only a qualified clinician can make an accurate diagnosis based on clinical assessment.
Borderline personality disorder test – MSI-BPD
The McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD) is a 10-item measure that was designed to screen for symptoms of BPD.
This test has good internal consistency and validity. It has been shown to be an effective tool for screening for BPD in clinical and research settings. Please note that no test will definitively diagnose borderline personality disorder. This instrument can help identify whether a person meets the criteria for a BPD diagnosis and provide information about symptom severity.
If you’re concerned that you or someone you know may have BPD, please reach out to a qualified mental health professional for further assessment and treatment.
Associated mental health problems
People with BPD may also have comorbid mental health conditions:
- Generalized anxiety disorder
- Bipolar disorder
- Depression
- Substance use disorders
- PTSD
- ADHD
- Eating disorders
- Dissociative disorders
- Other personality disorders
Other personality disorders and borderline personality disorder may be confused since they have certain symptoms in common. That’s why sometimes it’s difficult to distinguish the features and diagnose disorders accurately.
However, a person can be diagnosed with more than one personality disorder if they meet the criteria.
It’s especially common for people with borderline personality disorder to be misdiagnosed with bipolar disorder and vice versa because of symptomatic overlap.
How is BPD different from bipolar disorder?
- Borderline personality disorder is a personality disorder, while bipolar disorder is a mood disorder.
- Mood swings in BPD and bipolar disorder have different durations. For example, in people with bipolar disorder, depressive episodes may be much longer than in people with BPD.
- A bipolar person, between episodes of mania or depression, can demonstrate stability in daily functioning and relationships, which is not typical for BPD.
- BPD has psychological aspects, while bipolar disorder is more rooted in biological ones.
- In bipolar disorder, environmental changes have no impact on moods — e.g., a positive event can’t lift a depressed mood, while in borderline personality disorder, it can significantly impact the mood.
Borderline personality disorder treatments
The truth is, many people who experience borderline personality disorder symptoms don’t know that they have it. There is a lot of misinformation about it, and it’s important for them to get the right help they need and deserve.
For this reason, it is especially important to have a support system of family, friends, and healthcare professionals who are on hand to help you cope with the symptoms.
Borderline personality disorder is treatable, and recovery takes time. While there is no absolute cure, there are many ways that people with this disorder can deal with the symptoms and lead happy, stable, and healthy lives.
If left untreated, BPD can be devastating not only to the person but also to their loved ones.
So, what are the treatment approaches?
- Psychotherapy
- Self-care activities (journaling, meditation, mindfulness, regular exercising, healthy diet, quality sleep, developing social support, etc.)
- Medications
Medications
Currently, there are no FDA-approved medications for BPD treatment. But some medications can help reduce certain symptoms of this disorder and co-existing ones (depression, anxiety, etc.):
- Mood stabilizers
- Antidepressants
- Antipsychotics
- Anxiolytics
To develop the best strategy to get the symptoms under control, see your doctor and mental health professional.
Note that medication treatment alone often doesn’t work effectively. It doesn’t address negative behavior or thinking patterns. It should be used in conjunction with talk therapy.
Therapy for BPD
Psychotherapy is the fundamental treatment for dealing with borderline personality disorder.

People with BPD may experience intense emotions and impulsiveness lifelong. However, those who undergo therapy often show improvements from the 1st year and successfully stabilize their relationships by their 30s-40s.
There are some effective evidence-based approaches to treating borderline personality disorder:
Dialectical behavior therapy (DBT)
The DBT approach aims to teach:
- Coping skills
- How to control intense emotions
- Manage distress
- Reduce self-destructive behaviors
- Improve relationships
It’s focused on mindfulness and teaching how thoughts can lead to actions.
DBT helps people identify their capabilities, thus increasing their ability to regulate emotions and cope with the challenges they face in everyday life. DBT is often used to treat people with a high risk of self-harm and suicide.
DBT is a form of cognitive-behavioral therapy (CBT). It helps to change the way of thinking in order to change mood and behavior.
Together with the therapist, a person works to identify negative thinking patterns and behavioral responses to difficult situations. They develop more balanced and constructive ways to respond to challenges.
Schema therapy
The name of the approach emphasizes the idea that the person with BPD acts according to a schema formed in childhood. Such a schema may be formed under the influence of traumatic events or mistreatment and is activated in adulthood, provoking a certain perception of the world and reactions to it.
The goal of schema therapy is to help the person become aware of their schema, embrace it instead of adopting a new model, and find healthy ways to react to events by changing maladaptive behavior patterns.
Mentalization-based therapy (MBT)
MBT refers to the ability of people to reflect on and understand their and others’ feelings, emotions, and beliefs. It helps in:
- Learning emotion regulation skills
- Understanding how a person impacts their life events, problems, and relationships with others
- Understanding others and developing compassion for them
Transference-focused psychotherapy (TFP)
The goal of TFP is to help the person become aware of this cognitive distortion, develop a more stable and realistic self-image and perception of others, and learn to treat others in a healthier way through transference.
At Calmerry, we have available therapists trained in all the approaches above. We can match you with one of them within 1 hour – just start with a brief survey.
Conclusion
Borderline personality disorder is a serious mental health illness. The symptoms people with BPD experience every day are devastating for them and can significantly affect the lives of their loved ones. They need understanding and support from people around and qualified help from healthcare professionals.
If you think that you or someone you love may have a borderline personality disorder, see a psychiatrist or psychotherapist. Only they can make an accurate diagnostic assessment.
BPD is treatable, although it takes time and effort. You can reduce the impact of borderline personality disorder on your life by:
- Addressing traumatic events
- Learning healthy ways of dealing with emotions
- Speaking up about your problem and experiences
- Learning how to understand yourself and others better, etc.
Also, you can change your daily routines and practice self-care to control more aspects of your well-being. Seek a strong support system and professional help from an online therapist on Calmerry.
You deserve to live a healthy, happy life!
online therapy
live video session