What Is Clinical Depression and How Is It Treated?

In this article
Everyone has occasional down days, and it’s okay – it’s a normal part of life. But how can you tell if you’re experiencing a low mood or a medical condition like depression?
Clinical depression is also called a major depressive disorder, characterized as unipolar depression, with no “up” periods, only “down” periods. This guide will cover what clinical depression is, the signs and symptoms, its causes, and where to get help. We’ll also provide some top self-care tips for those with depression to help them manage their symptoms and aid recovery.
What is clinical depression itself?
Clinical depression is a serious, severe mental condition that affects how you feel, think, and act. As a result, people with clinical depression cannot function as well as they usually do in their daily life.
While we can all feel low or sad at various points in our lives, this doesn’t necessarily mean we have “clinical” depression. Clinical depression is defined as a severe form of depression that requires diagnosis and treatment. It can persist for weeks, months, or even years; you don’t feel better in just a few days, as with regular periods of sadness and apathy.
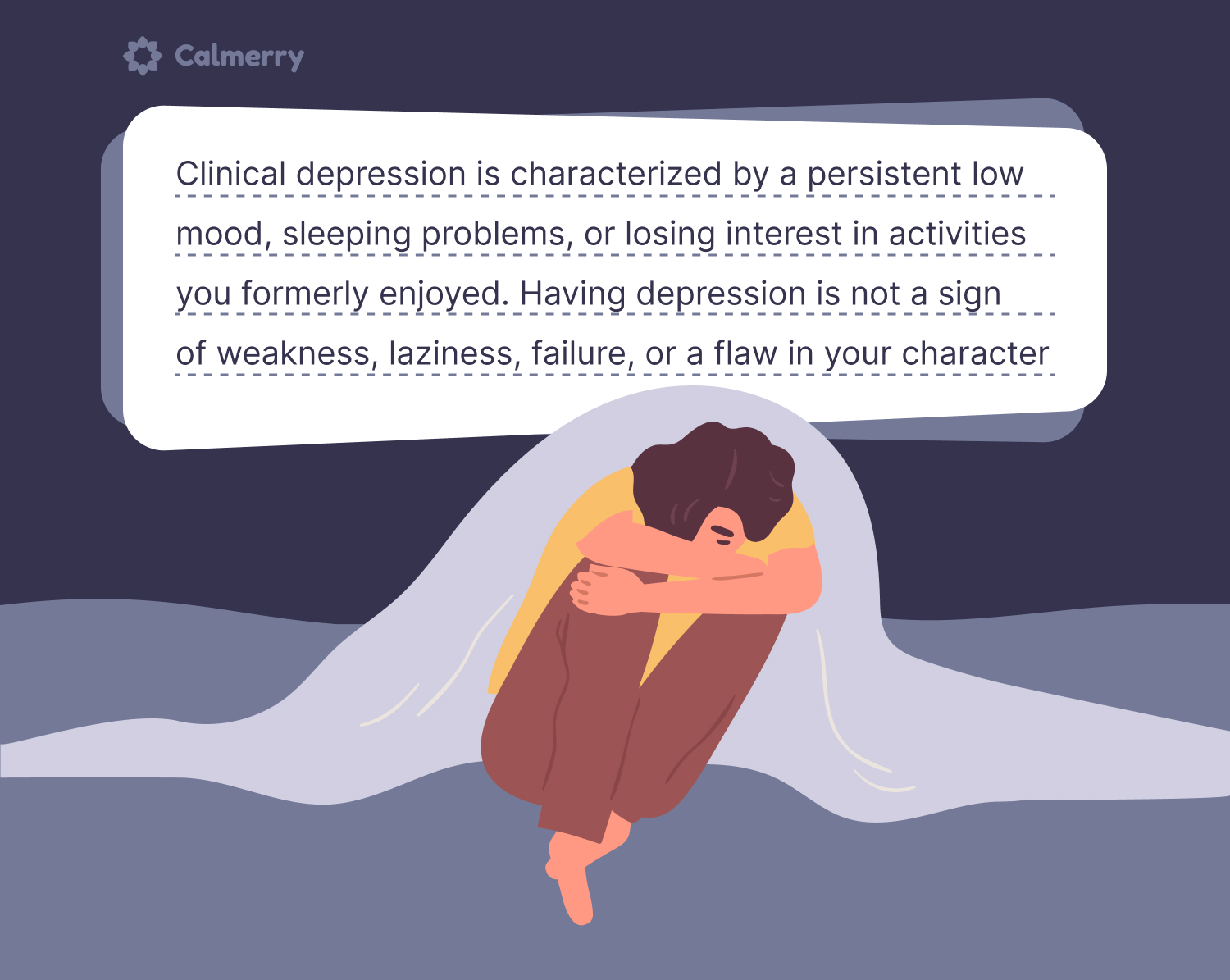
Clinical depression is characterized by a persistent low mood, sleeping problems, or losing interest in activities you formerly enjoyed. Having depression is not a sign of weakness, laziness, failure, or a flaw in your character. However, the symptoms of depression must affect you most days, for most of the day, and for at least two weeks to meet the criteria of clinical depression.
Depression affects people of all genders, ages, cultures, and ethnicities. According to WHO, more than 280 million people globally have depression.
Subtypes of clinical depression
In terms of clinical depression, there are several types, with the primary difference being the features involved. Here are some common subtypes of clinical depression:
- Anxious Depression: an MDD with anxiety-like symptoms.
- Melancholic Depression: a form characterized by persistent depression regardless of circumstances and worsens in the morning.
- Postpartum Depression (PPD): a form of major depression that women and some men experience within four weeks after having a baby.
- Psychotic Depression (PMD): a form of major depression with psychotic symptoms, such as hallucinations, delusions, and paranoia.
- Atypical Depression: a form which is characterized by mood-improving after positive circumstances or events, unlike classic MDD.
- Seasonal Affective Disorder (SAD): a form of major depression that happens only during certain seasons, most commonly during winter.
What are the symptoms of clinical depression?
The symptoms of clinical depression can vary from one person to another. However, it typically involves a persistent depressed mood or a loss of interest or pleasure in activities you usually enjoy.
Symptoms are also severe enough to affect your everyday life and functioning, causing work, family, or social difficulties. Here are some of the most common symptoms of major depressive disorder:
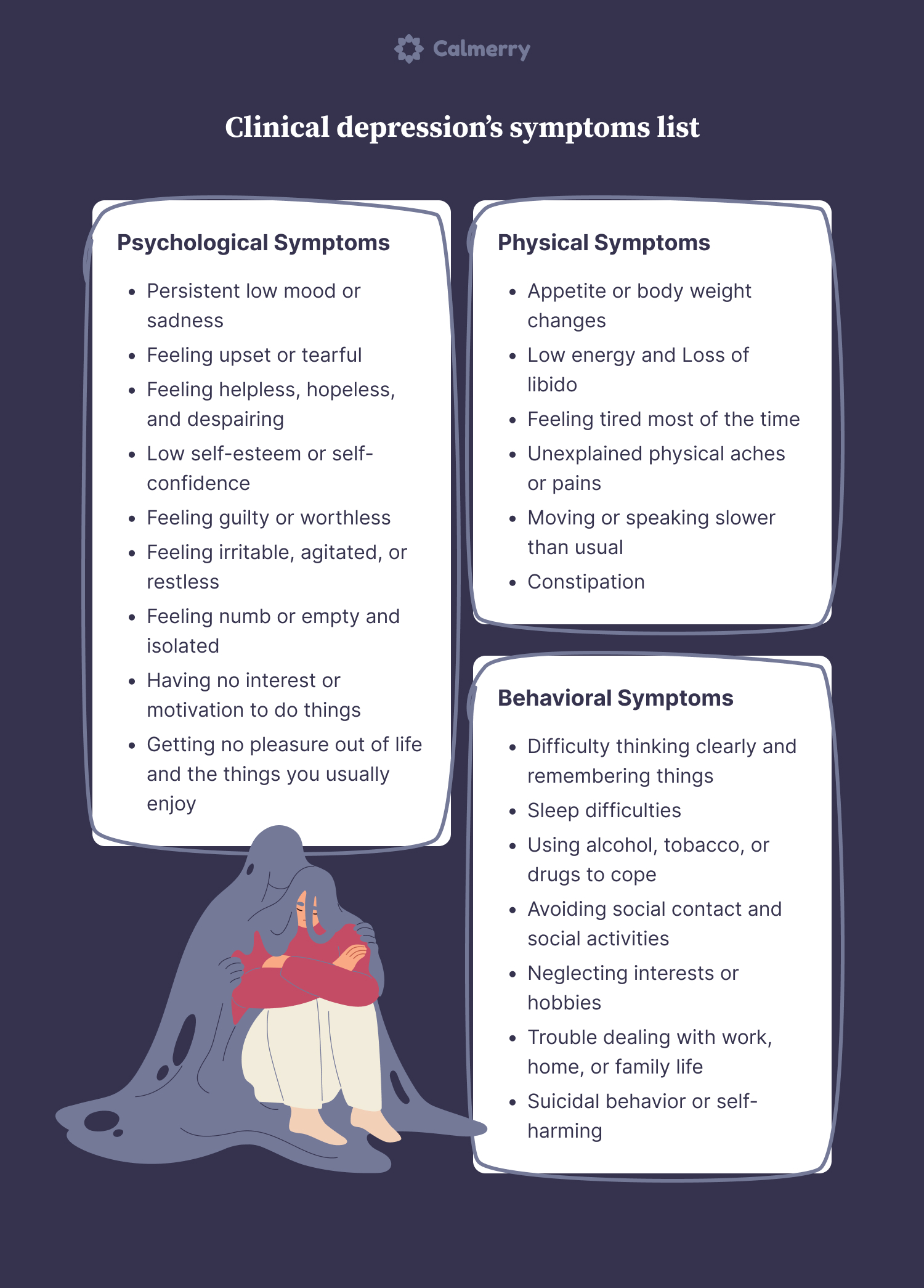
Psychological symptoms
The psychological symptoms of MDD may include:
- Persistent low mood or sadness
- Feeling upset or tearful
- Feeling helpless, hopeless, or despairing
- Low self-esteem or self-confidence
- Feeling guilty or worthless
- Feeling irritable, agitated, or restless
- Feeling numb or empty
- Feeling isolated
- Having no interest or motivation to do things
- Getting no pleasure out of life and the things you usually enjoy
- Worrying or feeling anxious
- Feeling suicidal or having thoughts of harming yourself
Physical symptoms
The physical symptoms of MDD may include:
- Appetite or body weight changes
- Low energy
- Feeling tired most of the time
- Unexplained physical aches or pains
- Moving or speaking slower than usual
- Loss of libido (sex drive)
- Constipation
Behavioral symptoms
The behavioral symptoms of MDD may include:
- Difficulty making decisions or thinking clearly
- Difficulty concentrating or remembering things
- Difficulty sleeping or oversleeping
- Using alcohol, tobacco, or drugs to cope
- Avoiding contact with others and social activities
- Neglecting interests or hobbies
- Trouble dealing with work, home, or family life
- Suicidal behavior or self-harming
Depression and suicide
Estimates show that around 60% of suicides are linked to mental health disorders like major depression and bipolar disorder. Having clinical depression can increase the risk of self-harm or suicide, especially when it’s left untreated.
If you are having suicidal thoughts, please get in touch with a doctor, emergency services, or a suicide prevention helpline right away.
What causes clinical depression?
What causes clinical depression is still not fully understood. However, it’s believed that various possible causes and factors may make a person more likely to develop depression.
Often, multiple factors can combine and trigger depression. The term “downward spiral” is often used to describe a series of adverse events that worsen your mental well-being and eventually lead to depression.
For example, if you’re going through a stressful divorce, you may drink more alcohol to cope, leading to work issues. All these things combined make you feel progressively worse until you become clinically depressed.
However, it’s also worth noting that some people can develop clinical depression without any obvious reasons.
Research suggests that the following are some of the most common causes of major depression:
- Life events: This includes traumatic or stressful events such as the death of a loved one, job loss or unemployment, divorce or separation, financial issues, bullying, and physical or sexual assault.
- Childhood trauma: This includes difficult or traumatic experiences in childhood, such as sexual, emotional, or physical abuse, neglect, household dysfunction, and family conflict.
- Personality: Certain personality traits or thought patterns such as self-criticism, overly pessimistic thinking, low self-esteem, perfectionism, and negative rumination may make you more likely to develop depression.
- Family history and genetics: You are more likely to develop depression if someone in your close family has had it before. This could be because of inherited genetics or through learned behavior from people around you.
- Health issues: Poor health, such as life-threatening illnesses, severe injuries, or chronic health problems that affect daily life, can increase your risk of becoming clinically depressed.
- Drug usage: A history of excessive alcohol or recreational drug misuse may cause or increase the likelihood of developing depression.
When to seek professional help
If you think you may have MDD or have experienced symptoms most days for more than two weeks, you should seek help from a doctor or licensed therapist.
Many people deal with depression alone and unnecessarily suffer for long periods before seeking help. However, it’s better not to delay; the sooner you get treatment, the quicker you’ll be able to feel better.
Clinical depression is a treatable condition, but it’s not something people can usually overcome alone. Also, depression can continue to worsen when it’s left untreated.
You can take this professional depression screening test if you experience symptoms of depression.
However, only a licensed therapist can come up with an accurate diagnosis. So, the best solution is to discuss the test results with a therapist who can help you address your feelings and develop a comprehensive treatment plan.
How to treat clinical depression
Psychotherapy and medication are the two main types of treatment for clinical depression:
Psychotherapy
Psychotherapy, also known as talking therapies, can effectively treat clinical depression. In our previous post, we talked about the most common types of talking therapy used for depression. Quick overview here:
- Cognitive Behavioral Therapy (CBT) – is a skills-based treatment for depression that focuses on changing your thought and behavior patterns.
- Interpersonal Therapy (IPT) – is a structured, short-term psychotherapy for depression that focuses on your relationships
- Psychodynamic Psychotherapy – is insight-oriented therapy and involves looking back into your childhood to help you understand yourself
- Dialectical behavior therapy (DBT) – is a mindfulness-based psychotherapy that teaches nonjudgmental, present-moment awareness to better cope with challenging feelings, including deep suffering.
Psychotherapy enables you to share your experiences in a confidential, safe, and non-judgmental environment. You can have psychotherapy one-on-one with a therapist or group, either in-person or online.
Your therapist can help you recognize your thoughts, emotions, and behaviors and understand how they affect your depression. Then, they can help you develop effective coping mechanisms and strategies to overcome your depression.
Medications
There are many types of antidepressants available for treating clinical depression, including:
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Tricyclics
- Monoamine Oxidase Inhibitors (MAOIs)
Antidepressants can be very effective, but they must be prescribed by a doctor or health professional. You may have to try different types, dosages, and combinations to find out what works best.
Antidepressants help millions of people manage their symptoms and improve their quality of life. However, it’s important to note that they do not work for everyone, and there can sometimes be issues with side effects.
Self-care tips for dealing with clinical depression
There are some things you can do to help improve your mood and aid recovery if you’ve been diagnosed with depression. Here are some top suggestions to explore for managing and easing depression.
Avoid unhealthy temptations and talk it out.
The use of alcohol and drugs might seem tempting when you’re depressed, as they can provide some immediate relief. However, they are unhealthy coping methods that can harm your health and make you feel much worse in the long run.
Sharing your experiences with someone you trust or a support group can provide valuable support and help you feel better. It also allows you to see things from another perspective and lifts the stress burden and isolation of coping alone.
Have a daily schedule and stick to a treatment plan.
You’re more likely to do an activity if you plan for it in advance and follow a daily schedule. Therefore, it helps you overcome the lethargy, lack of motivation, and avoidance behaviors often caused by depression. It also allows you to regain interest in activities you once enjoyed.
It’s important to take any medications prescribed, attend all therapy sessions scheduled, and follow any other advice given by your doctor or therapist.
Eat healthily and exercise
Regular physical activity can boost your mood, relieve stress, raise self-esteem, and trigger feeling-good endorphins. It can also help distract you from negative thoughts.
Like sports, eating healthy can lift your mood and improve your physical and mental health. Improving your diet can boost your energy levels and help you think more clearly.
Try journaling and mindfulness
Vent frustrations in a mood diary, record how you feel, what you think, and what worked in managing the symptoms. Thus, you’ll be able to track your emotions and feelings, notice changes in your mood, and recognize triggers and warning signs of your depressive episodes.
By practicing mindfulness, you can stop focusing on negative, depressive thoughts.
It is possible to gain control over them and react more healthily next time by learning to distance yourself from them through mindfulness.
Therapy can help
Clinical depression is a severe but sadly common illness. For those suffering from it, while there are many things you can do to help yourself, the best advice is always to seek professional help first. Speaking with and receiving treatment from a health professional is the surest way to get yourself on the path to recovery.
If you’d like to talk with one of our licensed therapists online at Calmerry, please get in touch – and we’ll match you with a professional within 1 hour. They can provide support and offer evidence-based treatments like cognitive behavioral therapy. We conduct all therapy sessions in a completely safe and confidential environment.
online therapy
live video session