CBT vs. DBT: Key Differences and Benefits

In this article
When it comes to types of therapy, it can be difficult to make sense of all the acronyms. CBT, ACT, DBT, EMDR… What are the differences among this alphabet of approaches, and which is right for you?
This article will focus on two popular approaches, cognitive-behavioral therapy (CBT) and dialectical behavioral therapy (DBT). While both fall under the umbrella of behavioral therapies, there are some key differences between the two.
What is CBT?
CBT is a type of talk therapy that combines principles from two branches of psychology: behaviorism and cognitive therapy.
The core principle of behaviorism is that rewards and consequences shape our actions, while cognitive therapists focus on the interplay among thoughts, emotions, and behaviors.
CBT integrates these two approaches, helping you to identify negative thoughts and behaviors and replace them with more adaptive ones.
What is DBT?
DBT incorporates many of the same philosophies of CBT but focuses on building skills to help you tolerate difficult emotions.
DBT traditionally occurs in a group setting but can be adapted to 1:1 therapy sessions. A DBT therapist will likely focus on the four areas of mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance.
What is the difference between CBT and DBT?
CBT and DBT both aim to help you find a better quality of life by managing negative emotions and changing maladaptive behaviors. Both therapies are structured and likely to include homework assignments to complete between sessions.
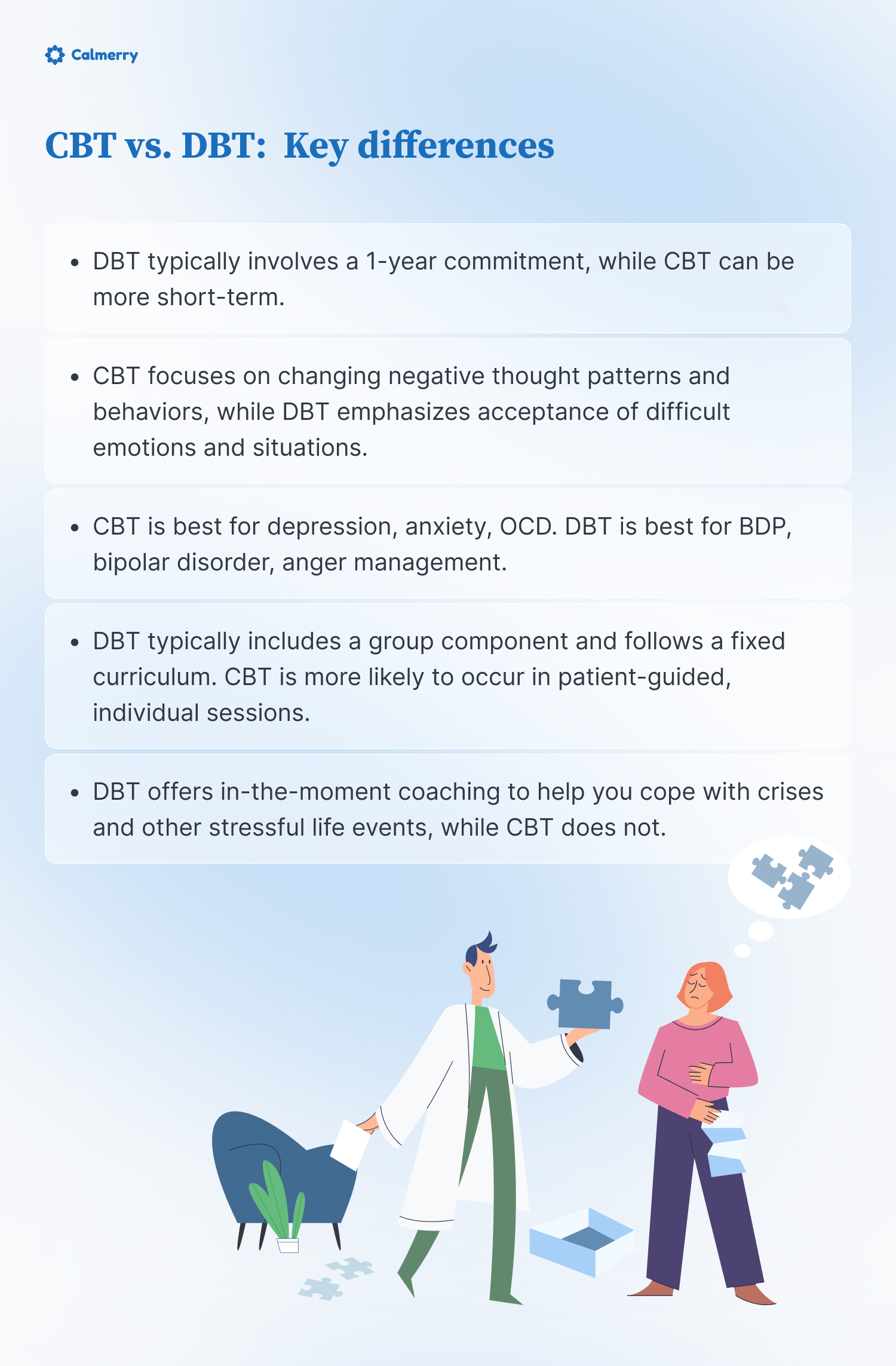
However, there are some important differences between CBT and DBT, including:
- DBT typically involves a 1-year commitment, while CBT can be more short-term.
- CBT focuses on changing negative thought patterns and behaviors, while DBT emphasizes acceptance of difficult emotions and situations.
- DBT typically includes a group component and follows a fixed curriculum. CBT is more likely to occur in patient-guided, individual sessions.
- DBT offers in-the-moment coaching to help you cope with crises and other stressful life events, while CBT does not.
CBT and DBT also differ in their core principles, issues treated, and techniques used. But before we delve into these areas, let’s review the historical background of DBT vs. CBT.
Historical background
Origin of CBT
CBT was developed in the 1960s by psychiatrist Aaron Beck. Dr. Beck started out researching psychoanalysis as a treatment for depression.
However, when the results of his work seemed to contradict psychoanalytic theory, Dr. Beck proposed a new model of depression. Dr. Beck found that by helping people change negative thought patterns and maladaptive behaviors, he could help them feel better and achieve a better quality of life.
Emergence of DBT
DBT was created by psychologist Marsha Linehan in the 1980s. It was originally a treatment for borderline personality disorder or BPD.
However, DBT has since been adapted to treat a range of issues. It is a particularly effective treatment approach for individuals struggling with emotion regulation, self-harm, or suicidal behaviors.
Core principles
CBT
The core principle of CBT is that our thoughts, feelings, and behaviors are interconnected. CBT focuses on replacing negative thought patterns with more realistic and positive ones.
For instance, a CBT therapist might help you to recognize faulty assumptions that you make about yourself, others, and the world. By identifying and challenging these beliefs, CBT can help you manage emotions, change maladaptive behaviors, and improve your overall mental health and well-being.
DBT
The word “dialectical” in dialectical behavioral therapy refers to the existence of two seemingly contradictory core principles: acceptance and change.
DBT teaches radical acceptance, a skill based on the belief that our resistance to pain creates suffering. DBT also uses mindfulness to help you change the way you respond to intense emotions.
The ultimate goal of DBT is to help you create a “life worth living” by managing your emotions more effectively.
Who is it for?
Both CBT and DBT are used to treat a variety of mental health issues.
However, CBT tends to work better for people who struggle with negative thought patterns, while DBT is often more effective for those who struggle with emotion regulation and impulse control.
Here is a list of mental health conditions that CBT and DBT can address:
CBT
- Depression
- Anxiety disorders
- Post-traumatic stress disorder (PTSD)
- Obsessive-Compulsive Disorder (OCD)
- Eating disorders
- Substance use disorders
- Stress-related disorders
DBT
- Borderline personality disorder (BPD)
- Self-harm and suicidal behaviors
- Substance use disorders
- Anger management
- Attention-deficit hyperactivity disorder (ADHD)
- Bipolar disorder
- Post-traumatic stress disorder (PTSD)
- Eating disorders
Both CBT and DBT therapists will tailor treatment to meet your specific needs, possibly combining elements of both approaches. Additionally, these therapies are not limited to the issues listed above and can be applied to other psychological challenges.
Techniques used
CBT techniques
CBT is a collaborative, goal-oriented approach that encourages you to take an active role in therapy. It often begins with identifying a specific problem you want to resolve – for example, “I want to stop worrying so much.”
Your therapist will then help you work towards this goal using a variety of strategies, including:
- Cognitive restructuring – identifying and challenging negative or irrational thought patterns and replacing them with more realistic ones
- Exposure therapy – gradually approaching the object or situation that you fear in a safe and controlled environment
- Behavior activation – identifying activities that you have stopped doing because of depression or anxiety and gradually reintroducing them into your daily routine
DBT techniques
DBT teaches concrete skills to help you manage intense emotions, improve interpersonal skills, and build “a life worth living.”
These techniques include:
- Mindfulness skills – observing what is happening, describing your experience, and fully engaging in the present moment
- Interpersonal effectiveness – achieving your goals in a situation while improving relationships and maintaining self-respect
- Emotion regulation – putting words to your emotions, checking the facts of the situation, and identifying more effective ways to respond
- Distress tolerance – engaging in positive activities, imagery, prayer, and relaxation to cope with difficult situations
Evidence and effectiveness
CBT
Research shows that CBT is an effective therapy for a variety of conditions, including physical ailments like fibromyalgia and irritable bowel syndrome. [1] Nakao, M., Shirotsuki, K., & Sugaya, N. (2021). Cognitive–behavioral therapy for management of mental health and stress-related disorders: Recent advances in techniques and technologies. BioPsychoSocial Medicine, 15(1). https://doi.org/10.1186/s13030-021-00219-w
CBT is particularly successful as a treatment for depression. A recent analysis of 115 studies found that CBT effectively reduced the symptoms of mild to moderate depression. [2] Gautam, M., Tripathi, A., Deshmukh, D., & Gaur, M. (2020). Cognitive Behavioral therapy for depression. Indian Journal of Psychiatry, 62(8), 223. https://doi.org/psychiatry_772_19 Patients who received CBT also were less likely to relapse than patients who received medication alone.
CBT also provides long-term benefits for patients with generalized anxiety disorder, social anxiety disorder, and post-traumatic stress disorder. [3] Van Dis, E. A., Van Veen, S. C., Hagenaars, M. A., Batelaan, N. M., Bockting, C., Van Den Heuvel, R. M., Cuijpers, P., & Engelhard, I. M. (2020). Long-term Outcomes of Cognitive Behavioral therapy for Anxiety-Related Disorders. JAMA Psychiatry, 77(3), 265. https://doi.org/10.1001/jamapsychiatry.2019.3986 A 2021 study of primary care patients found that CBT significantly improved symptoms of mild to moderate anxiety. [4] Bogucki, O. E., Craner, J. R., Berg, S. L., Wolsey, M. K., Miller, S., Smyth, K. T., Johnson, M., Mack, J. D., Sedivy, S. J., Burke, L., Glader, M. A., Williams, M. W., Katzelnick, D. J., & Sawchuk, C. N. (2021). Cognitive Behavioral Therapy for Anxiety Disorders: Outcomes from a Multi-State, Multi-Site Primary Care practice. Journal of Anxiety Disorders, 78, 102345. https://doi.org/10.1016/j.janxdis.2020.102345
Finally, CBT is considered a first-line therapy for OCD, with between 50% and 70% of patients responding to treatment. [5] O’Neill, J., & Feusner, J. D. (2015). Cognitive-behavioral therapy for obsessive–compulsive disorder: access to treatment, prediction of long-term outcome with neuroimaging. Psychology Research and Behavior Management, 211. https://doi.org/10.2147/prbm.s75106 As with depression, patients receiving CBT are less likely to experience a recurrence of symptoms than patients treated with medication alone.
DBT
While some studies have shown DBT to be effective in treating depression and anxiety, there is more evidence for CBT. Thus, CBT might be a better option for people with these conditions.
In contrast, DBT is more effective at treating borderline personality disorder (BPD). In fact, DBT is the only empirically validated treatment for BPD, meaning that BPD patients who receive DBT have significantly higher rates of recovery than patients who receive other therapies. [6] May, J. M., Richardi, T. M., & Barth, K. S. (2016). Dialectical behavior therapy as treatment for borderline personality disorder. The Mental Health Clinician, 6(2), 62–67. https://doi.org/10.9740/mhc.2016.03.62
Evidence also suggests that DBT is more effective than CBT for the treatment of bipolar disorder. A recent study of 60 patients with bipolar depression found that DBT significantly reduced symptoms, improving emotion regulation and executive functioning skills like memory and attention. [7] Afshari, B., Omidi, A., & Ahmadvand, A. (2019). Effects of dialectical behavior therapy on executive functions, emotion regulation, and mindfulness in bipolar disorder. Journal of Contemporary Psychotherapy, 50(2), 123–131. https://doi.org/10.1007/s10879-019-09442-7
Finally, research indicates that DBT may be better than CBT for the treatment of eating disorders. While there is the most evidence supporting DBT as a therapy for binge eating disorder, preliminary studies suggest that DBT could be effective in treating bulimia and anorexia, as well. [8] Ben-Porath, D. D., Duthu, F., Luo, T., Gonidakis, F., Compte, E. J., & Wiśniewski, L. (2020). Dialectical behavioral therapy: an update and review of the existing treatment models adapted for adults with eating disorders. Eating Disorders, 28(2), 101–121. https://doi.org/10.1080/10640266.2020.1723371
So, what to choose?
CBT is more widely used and has more research supporting its efficacy. However, which therapy is right for you depends on your individual needs, preferences, and circumstances.
Here are some things to consider when deciding between CBT and DBT:
- What do you want help with? If you’d like to focus on changing negative thought patterns, you might benefit from CBT. If you want to improve emotion regulation, DBT may be a better fit.
- Do you prefer your therapist to act like a coach, teaching you concrete skills you can use outside of sessions? If so, DBT might work for you.
- Do you need your therapist to be readily available in times of crisis? While some CBT therapists offer after-hours communication, this is more typical with DBT.
- How do you feel about group work? DBT often includes a group component.
- How do you feel about mindfulness? If the thought of sitting with your thoughts and feelings turns your stomach, you might find DBT challenging to stick with.
- How much time can you commit to therapy? DBT requires a greater time commitment, while CBT can be more short-term and time-limited.
Still on the fence? A licensed mental health professional can help you determine which treatment is right for you.
While there may be comparably more therapists trained in CBT, online therapy gives you access to clinicians with a wide variety of backgrounds and certifications, including those with DBT training.
Seek CBT or DBT online
At Calmerry, we have over 1000 mental health professionals who can provide help for various mental health issues and conditions. They use different therapeutic approaches, including CBT and DBT, and we can match clients within 1 hour with their best-fit professional.
Clients start with a brief survey that helps our agents understand their needs more. Clients can change therapists anytime they feel like it.
Nakao, M., Shirotsuki, K., & Sugaya, N. (2021). Cognitive–behavioral therapy for management of mental health and stress-related disorders: Recent advances in techniques and technologies. BioPsychoSocial Medicine, 15(1). https://doi.org/10.1186/s13030-021-00219-w
Gautam, M., Tripathi, A., Deshmukh, D., & Gaur, M. (2020). Cognitive Behavioral therapy for depression. Indian Journal of Psychiatry, 62(8), 223. https://doi.org/psychiatry_772_19
Van Dis, E. A., Van Veen, S. C., Hagenaars, M. A., Batelaan, N. M., Bockting, C., Van Den Heuvel, R. M., Cuijpers, P., & Engelhard, I. M. (2020). Long-term Outcomes of Cognitive Behavioral therapy for Anxiety-Related Disorders. JAMA Psychiatry, 77(3), 265. https://doi.org/10.1001/jamapsychiatry.2019.3986
Bogucki, O. E., Craner, J. R., Berg, S. L., Wolsey, M. K., Miller, S., Smyth, K. T., Johnson, M., Mack, J. D., Sedivy, S. J., Burke, L., Glader, M. A., Williams, M. W., Katzelnick, D. J., & Sawchuk, C. N. (2021). Cognitive Behavioral Therapy for Anxiety Disorders: Outcomes from a Multi-State, Multi-Site Primary Care practice. Journal of Anxiety Disorders, 78, 102345. https://doi.org/10.1016/j.janxdis.2020.102345
O’Neill, J., & Feusner, J. D. (2015). Cognitive-behavioral therapy for obsessive–compulsive disorder: access to treatment, prediction of long-term outcome with neuroimaging. Psychology Research and Behavior Management, 211. https://doi.org/10.2147/prbm.s75106
May, J. M., Richardi, T. M., & Barth, K. S. (2016). Dialectical behavior therapy as treatment for borderline personality disorder. The Mental Health Clinician, 6(2), 62–67. https://doi.org/10.9740/mhc.2016.03.62
Afshari, B., Omidi, A., & Ahmadvand, A. (2019). Effects of dialectical behavior therapy on executive functions, emotion regulation, and mindfulness in bipolar disorder. Journal of Contemporary Psychotherapy, 50(2), 123–131. https://doi.org/10.1007/s10879-019-09442-7
Ben-Porath, D. D., Duthu, F., Luo, T., Gonidakis, F., Compte, E. J., & Wiśniewski, L. (2020). Dialectical behavioral therapy: an update and review of the existing treatment models adapted for adults with eating disorders. Eating Disorders, 28(2), 101–121. https://doi.org/10.1080/10640266.2020.1723371
online therapy
live video session